ISSN: 0973-7510
E-ISSN: 2581-690X
https://dx.doi.org/10.22207/JPAM.13.1.65 | © The Author(s). 2019
Nosocomial or hospital acquired infections are acquired by the patients during hospital stay. Bacteria were found to be responsible for the majority of infections followed by fungi, viruses, and protozoa. Literature has demonstrated that hospitals with infection control guidelines help reduce infection rates. We therefore isolated and compared common nosocomial organisms causing infections previous to and after the implementation of infection control measures to control healthcare-associated infections in our hospital setting. Strategy for infection control in our hospital setting was devised in the year 2010. These guidelines were frequently revised to improve the compliance of infection control measures. Infection control nurse helped record all the positive cultures in a surveillance format. This data on the number of isolates recovered from the cultures was documented and compared each year to check for the compliance of the infection control guidelines to reduce microbial isolates causing infections. Of the recovered 866 isolates from microbial cultures known to be causing nosocomial infections, 77.7% were gram-negative bacteria, 13.2% were gram-positive bacteria and 9% were fungi. A decrease in the number of microbes causing infections was observed after the implementation of infection control measures, with only 3.4% of the gram-positive microbes, 9.6% of the gram-negative microbes and 3.8% of the fungi being identified in the year 2017. Our study demonstrated that effectively devised infection control measures help reduce the number of organisms causing nosocomial infections further resulting in decreased infection rate.
Nosocomial Infections; Health Issues; Infection Control; Bacteria; Hospital Stay.
“Nosocomial or hospital-acquired infections” is the term used for any infection acquired by the patient during the hospital stay. In recent times, a new idiom, “healthcare-associated infections” is used for the type of infections caused by a prolonged hospital stay and is a major risk factor for serious health issues leading to death (Khan et al. 2015). Developing countries account for a greater burden of these infections when compared to the developed countries.
Literature regarding studies conducted in different parts of the world revealed that 5-10% of all hospitalizations in North America and Europe result in nosocomial infections, whereas Latin America, Sub-Saharan Africa, and Asia demonstrated more than 40% hospitalizations with nosocomial infections (World Health Organization. 2002). Two pathophysiologic factors must be present for the development of a nosocomial infection; impaired host defenses and colonization by pathogenic and non-pathogenic bacteria.
The most part of infections arises from the endogenous bacterial flora although critically ill patients in due course become colonized with resistant bacterial strains (Agaba et al. 2017). Bacterial species account for almost 90% of the nosocomial infections, whereas fungi, viruses, and mycobacteria have a less contributing role compared to bacterial infections (Gatermann et al. 2005). The agents that are frequently responsible for hospital-acquired infections comprise of Streptococcus species, Acinetobacter, Enterococcus, Pseudomonas aeruginosa (P. aeruginosa), and Staphylococcus aureus (S. aureus) (Horan et al. 2008).
Keeping in mind the mortality, morbidity, prolonged hospital stay and the cost, efforts should be taken to make hospitals as safe as possible to prevent such infections. Data from a small number of facilities in India propose that the implementation of hospital infection measures is a feasible option to reduce infection rates (Jaggi et al. 2013, Mehta et al. 2013). Reports from the hospitals with an effective infection surveillance and control program revealed infection rates to be reduced by approximately one-third (Haley et al. 1985).
Formulation of these infection control guidelines depends both on the physician understanding of epidemiologic observations in intensive care units and their knowledge of findings in the microbiology laboratory (Ebnother et al. 2008). These guidelines help both the health care personnel involved in patient care and the persons responsible for the surveillance and management of infections in the hospital.
Since nosocomial infections can be caused by several organisms but few were found to be particularly responsible for hospital-acquired infections (HAIs) we isolated and compared common nosocomial organisms causing HAIs previous to and after implementation of infection control measures to control healthcare-associated infections in our hospital setting.
The discipline concerned with the prevention of nosocomial or healthcare-associated infection is infection control. Care hospital, Hyderabad has been a pioneer institution in managing infection control in our country. The present descriptive study involved identifying microbial isolates causing nosocomial infections from 2010-2017 and further evaluated their recovery from cultures after implementation of infection control measures in our hospital.
Ethical approval
Ethical approval was obtained from the Institutional Ethics Committee, Care Group of hospitals.
Agenda to initiate this programme was discussed in the hospital infection control committee meeting. Strategies to achieve infection control in our hospital setting was formulated by the infection control team in the year 2010 (Table 1) and were frequently revised each year to allow for improved compliance of the infection control measures.
Table (1):
Guidelines formulated by the Infection control committee
S. No |
Guidelines |
|---|---|
1. |
Physicians treating inpatients have to remove their aprons prior to their entry in the intensive care units (ICUs) |
2. |
An obligatoryrule to use shoe covers before entering the intensive care units |
3. |
To prevent transmission of infection between patients, stethoscope needs to be disinfected using alcohol swabs. |
4. |
Dry mops to be used in all the ICU’S by the hospital housekeepers |
5. |
As an alternative to saline wash, heplocks should be used to flush intravenous (IV) lines |
6. |
Cloth masks and caps to substitutedisposable caps and masks |
7. |
Provision of N-95 masks for every open case of tuberculosis |
8. |
Color coding stickers for recognition of infected patients |
9. |
Employspacers to nebulizepatients on ventilators |
10. |
All the housekeeping, nursing staff, and technicians in critical areas to be vaccinated against Hepatitis-B |
11. |
Customary monitoring of fumigation practices in the intensive care units |
12. |
Implementation of air sampling in the operation theatres and intensive care units |
13. |
Methicillin-resistant Staphylococcus aureus (MRSA) policy was executed and necessary precautions concerning it was given to all nursing station |
14. |
Mandatory reporting of extended-spectrum beta-lactamases in the microbiology lab |
15. |
All surgical instruments to be disinfected using Korsolex |
16. |
The institution of effective measures to improve hand hygiene practices |
17. |
Monitoring hygienic practices in the canteen to minimize the transmission of infections to the patients |
Apart from this needle stick injury policy was implemented and protocols for handling infected linen was circulated to all nursing stations. Auditing high end and reserved antibiotics to streamline their use were also performed as a part of the infection control measure. Separate places were identified for washing of dressing sets in all the nursing stations before sending it to the Central sterile service department (CSSD). Multivariable (MVI) indicators helped in the additional evaluation of the proper sterilization of the dressing sets.
Data regarding the isolation of specimens was collected through active surveillance by infection control nurses on an everyday basis and was documented in the surveillance format. It has been reported that the incidence of nosocomial infections in the intensive care unit (ICU) is about 2 to 5 times higher than in the general inpatient hospital population ( Ewans et al. 1999).
Table (2):
Illustrates isolates of gram-positive organisms causing nosocomial infections during the period 2010-2017
Gram positives |
2010
N (%) |
2011
N (%) |
2011
N (%) |
2012
N (%) |
2013
N (%) |
2014
N (%) |
2015
N (%) |
2016
N (%) |
2017
N (%) |
Total |
|---|---|---|---|---|---|---|---|---|---|---|
Enterococcus faecalis |
12 |
9 |
17 |
6 |
9 |
8 |
6 |
4 |
4 |
75 |
Enterococcus faecium |
12 |
9 |
0 |
6 |
0 |
0 |
0 |
0 |
0 |
27
|
Staphylococcus aureus |
0 |
3 |
0 |
1 |
3 |
2 |
3 |
1 |
0 |
13
|
Total |
24
(20.8%) |
21
(18.2%) |
17
(14.7%) |
13
(11.3%) |
12
(10.4%) |
10
(8.6%)
|
9
(7.8%) |
5
(4.3%) |
4
(3.4%) |
115 |
A total of 115 isolates of gram-positive organisms causing nosocomial infections were identified during the years 2010-2017 (Table2). A decrease in the number of isolates was seen from the year 2010 to 2017 with only 3.4% of them being identified in the year 2017. Among the gram-positive isolates, the most common organism identified was Enterococcus faecalis, followed by Enterococcus faecium and Staphylococcus aureus.
Henceforth, we collected data from the intensive care units i.e. neonatal intensive care unit (NICU), neurosurgery intensive care unit (NSICU), intermediate care unit (IMCU), intensive care cardiac unit (ICCU), medical intensive care unit (MICU), surgical intensive care unit (SICU), and cardiothoracic intensive care unit (CTICU) and subjected it to regular analysis. We furthermore conducted regular monthly programs on infection control practices to improve awareness among the physicians, nursing, and hospital housekeepers.
After an informed consent from the patients, appropriate clinical samples were collected and cultured for isolation/biochemical identification. For isolating the pathogens from the specimens we inoculated the specimens in common media which help in bacterial growth such as Blood agar, Chocolate agar, and Mac Conkey agar. Further incubation at 37°C for 24 hours promoted the growth of the microorganisms. The microscopically identified gram positive, gram negative microbes and fungi were additionally subjected to biochemical reactions to provide information on the species specificity.
Infection control nurse helped record all the positive cultures following which she obtained further data regarding the admission of the patient from the respective wards. This data on the number of isolates recovered from the cultures was documented and compared each year to check for the compliance of the infection control guidelines to reduce microbial isolates causing infections.
Statistical data
Data was compiled using Microsoft excel sheet. Descriptive statistics were used to calculate the number of isolates recovered from the cultures in terms of percentages.
In the present study, we checked for the compliance of our devised infection control guidelines to reduce the number of nosocomial organisms causing infection. We further categorized the isolated microbes into gram-positive bacteria, gram-negative bacteria and fungi to further our understanding on which category of organisms accounted for the most part of nosocomial infections (Fig. 1).
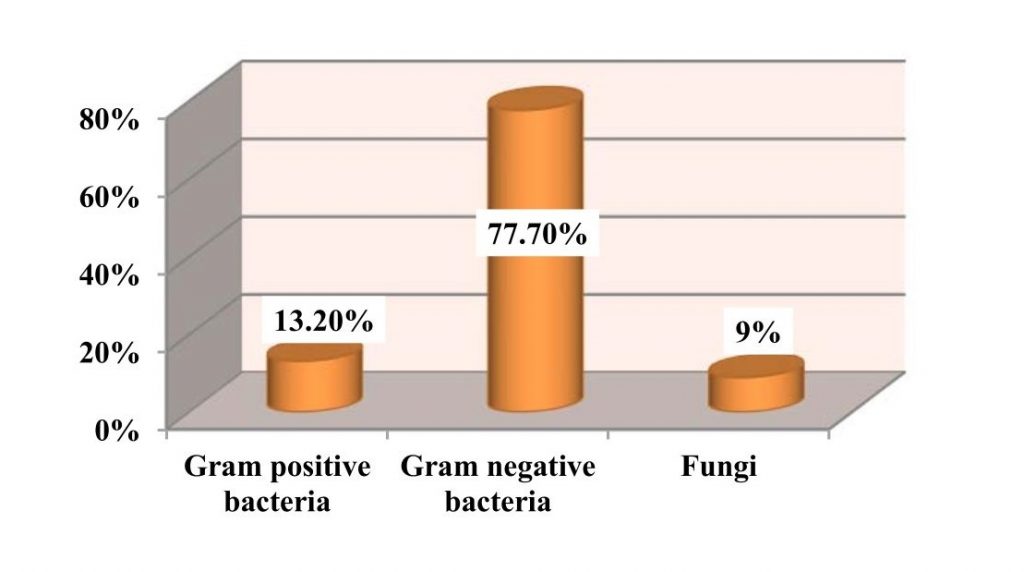
Fig. 1.Percentage of gram-positive, gram-negative and fungal organisms isolates recovered from the culture
Table (3):
Illustrates isolates of gram-negative organisms causing nosocomial infections during the period 2010-2017
Gram negatives |
2010 |
2011 |
2012 |
2013 |
2014 |
2015 |
2016 |
2017 |
Total |
|---|---|---|---|---|---|---|---|---|---|
Klebsiella Pneumoniae |
38 |
34 |
7 |
10 |
17 |
15 |
25 |
11 |
157 |
Pseudomonasaeruginosa |
30 |
26 |
16 |
24 |
16 |
14 |
12 |
12 |
150
|
Acinetobacter |
13 |
9 |
15 |
15 |
6 |
17 |
2 |
15 |
92
|
E.Coli ESBL
Extended-spectrum beta-lactamases |
30 |
12 |
27 |
22 |
25 |
19 |
17 |
16 |
168
|
Enterobacter |
6 |
7 |
17 |
13 |
5 |
3 |
10 |
5 |
66
|
Citrobacter koseri |
3 |
1 |
2 |
0 |
2 |
2 |
3 |
1 |
14
|
Proteus mirabilis |
2 |
2 |
1 |
0 |
1 |
0 |
1 |
2 |
9
|
Burkholderia |
1 |
1 |
0 |
0 |
2 |
1 |
3 |
1 |
9
|
Stenotrophomonas maltophilia |
2 |
1 |
1 |
0 |
0 |
2 |
0 |
2 |
8
|
Total |
125
(18.5%) |
93
(13.8%) |
86
(12.7%) |
84
(12.4%) |
74
(10.9%) |
73
(10.8%) |
73
(10.8%) |
65
(9.6%) |
673 |
A total of 673 isolates of gram-negative organisms causing nosocomial infections were identified during the years 2010-2017 (Table3). The number of gram-negative isolates reduced to 9.6% in the year 2017 in comparison to 18.5% isolates observed in the year 2010 when the infection control program began. Among the gram-negative isolates, the most commonly identified one was Escherichia coli Extended-spectrum beta-lactamases (E. coli ESBL), followed by Klebsiella pneumoniae, Pseudomonas, and Acinetobacter.
Of the recovered 866 isolates from microbial cultures known to be causing nosocomial infections, 673 (77.7%) were gram-negative bacteria, 115 (13.2%) were gram-positive bacteria and 78 (9%) were fungi.
Table (4):
Illustrates isolates of fungi causing nosocomial infections during the period 2010-2017.
Fungi |
2010 |
2011 |
2012 |
2013 |
2014 |
2015 |
2016 |
2017 |
Total |
|---|---|---|---|---|---|---|---|---|---|
Candida albicans |
12 |
9 |
11 |
8 |
4 |
1 |
1 |
1 |
47
|
Candida Tropicalis |
4 |
3 |
0 |
1 |
2 |
1 |
0 |
2 |
13
|
Candida
Krusie |
1 |
2 |
0 |
1 |
1 |
2 |
1 |
0 |
8
|
Candida glabrata |
1 |
1 |
0 |
2 |
1 |
3 |
1 |
0 |
9
|
Candida Parapsilosis |
1 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
1
|
Total |
19
(24.3%) |
15
(19.2%) |
11
(14.1%) |
12
(15.3%) |
8
(10.2%) |
7
(8.9%) |
3
(3.8%) |
3
(3.8%) |
78 |
The number of fungal organisms isolated from the intensive care units decreased to 3.8% in the year 2017 in contrast to the 24.3% isolates identified in the year 2010 (Table 4). Most commonly isolated fungal organisms were Candida albicans, Candida tropicalis and Candida krusie.
Hospital-acquired infections are a major concern equally for the health care providers and the patients. To combat these infections we devised infection control guidelines to evaluate if an appropriate infection controls guideline helps reduce the number of nosocomial organisms causing infection. In the present study, a total of 866 isolates were recovered from cultures with gram-negative organisms (77.7%) accounting for the majority of infections, followed by gram-positive microbes (13.2%), and fungi. Data from the intensive care units in the United States also reported that gram-negative bacteria account for 70% of the nosocomial infections (Gaynes et al. 2005).
The number of gram-positive organisms causing infections in our study decreased from 20.8% to 3.4%. Among the gram-positive isolates, the most common organism identified was Enterococcus faecalis, followed by Enterococcus faecium and Staphylococcus aureus. Enterococci are the most frequent causes of nosocomial infections, particularly in the intensive care units. They are frequently transmitted from person to person through the hands of hospital personnel and occasionally through medical devices (Olawale, 2011). A decrease in the number of Enterococcus isolates in the present study could be attributed to the improved hand hygiene measures and disinfection of surgical instruments implemented as a part of our infection control policy.
The number of gram-negative isolates reduced to 9.6% in the year 2017 in comparison to 18.5% isolates observed in the year 2010 when the infection control program began. E. coli ESBL was the most commonly isolated gram-negative pathogen in the present study followed by Klebsiella pneumoniae (K. pneumoniae), Pseudomonas, and Acinetobacter. Entero-bacteriaceae family constitutes the Klebsiella and Escherichia coli species. The high resistance to antibiotics by this group of microbial species constitutes one major reason for nosocomial infections (Khan et al. 2017). Antibiotic control policy to audit high end and reserved antibiotics use as a part of our infection control measure helped reduced the number of Enterobacteriaceae isolates in the present study.
The common pathogens causing infections i.e. ventilator-associated pneumonia include gram-negative bacteria such as Pseudomonas aeruginosa, Escherichia coli, K. pneumoniae, Acinetobacter species, and gram-positive microbe such as Staphylococcus aureus (Chi et al. 2012). A gradual decrease in the number of these microbial isolates was seen over a period of time from 2010-2017 after the implementation of infection control guidelines. The use of spacers to nebulize patients on ventilators, regular monitoring of fumigation practices, implementation of air sampling units in all the ICUs and other infection control measures might have accounted for this decrease in our present study.
Certain pathogens survive in the environment for an extended period of time, principally the Enterococcus and the Acinetobacter species. Environmental factors chiefly improper cleaning and disinfection have been found accountable for their survival leading to nosocomial infections (Mehta et al. 2014). Protocols for handling infected linen and washing of dressing sets, disinfection of all surgical instruments using Korsolex and additional cleaning and disinfection protocols accounted for this decrease of environmental pathogens.
In hospital settings, K. pneumonia is transmitted by person-to-person contact and in particularly when healthcare professionals do not wash or clean hands subsequent to checking a contaminated patient (Khan et al. 2015). Improvement of the hand hygiene helps minimize nosocomial infection as proposed by the World Health Organization (WHO) (Abdellatif et al. 2007). Hence the promotion of effective measures to improve hand hygiene by organizing training classes on hand washing practices and provision of hand washing facilities in all critical care areas and nursing stations accounted for this decrease as observed in the year 2017.
Pseudomonas aeruginosa tolerates a wide range of physical conditions, with minimal requirements for growth. In hospitals, it has been isolated from food, floor mops (moist environment promotes its growth), respiratory and dialysis equipment. It is an important nosocomial pathogen because of its intrinsic resistance to antimicrobials (Lim et al. 2005). A decrease in the number of P. aeruginosa isolates has been observed in the present study from (20%; 20/150) to (8%; 12/150). Infection control measures including the use of dry mops, monitoring hygienic practices in the canteen and streamlining high end and reserved antimicrobial use would have contributed to this decrease in the current study.
Apart from bacterial species, fungal organisms also act as opportunistic pathogens causing nosocomial infections in immune-compromised individuals (Ducel, 2002). Most commonly isolated fungal organisms in our present study were Candida albicans, Candida tropicalis, and Candida glabrata. Although C. albicans remains the most common cause of nosocomial infections a number of reports have documented infections caused by other Candida species: C. tropicalis, C. glabrata, and C. krusei which is in line with our current study (Pfaller, 1996).
In this era of antibiotics, nosocomial infections are still unmanageable. Our study revealed that an effectively devised infection control guideline helps reduce the number of organisms causing nosocomial infections. There is also a great need that best infection control practices be shared among hospitals to control the spread of these infections.
None
The authors declare that they have no conflict of interest.
- Khan HA, Ahmad A, Mehboob R. Nosocomial infections and their control strategies. Asian pacific journal of tropical biomedicine., 2015; 5(7):509-14.
- World Health Organization. Prevention of hospital-acquired infections: a practical guide. World Health Organization, Geneva (2002)
- Agaba P, Tumukunde J, Tindimwebwa JVB, Kwizera A. Nosocomial bacterial infections and their antimicrobial susceptibility patterns among patients in Ugandan intensive care units: a cross sectional study. BMC Research Notes., 2017; 10:349.
- Gatermann S, Funfstuck R, Handrick W, Leitritz L, Naber KG, Podbielski A, et al. [MIQ 02: Urinary Tract Infections: Quality standards for microbiological infections] Urban & Fischer, Munchen. 2005, 8-21.
- Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting Am. J. Infect Control, 2008; 36(5):309-332.
- Jaggi N, Rodrigues C, Rosenthal VD, et al. Impact of an international nosocomial infection control consortium multidimensional approach on central line-associated bloodstream infection rates in adult intensive care units in eight cities in India. Int. J. Infect Dis., 2013; 358.
- Mehta Y, Jaggi N, Rosenthal VD, et al. Effectiveness of a multidimensional approach for prevention of ventilator-associated pneumonia in 21 adult intensive-care units from 10 cities in India: findings of the International Nosocomial Infection Control Consortium (INICC). Epidemiol Infect., 2013; 358:2483-91.
- Haley RW, Culver DH, White JW, Morgan WM, Emori TG, Munn VP, et al. The efficacy of infection surveillance and control programs in preventing nosocomial infections in US hospitals. Am. J. Epidemiol., 1985; 121:182–205.
- Ebnother C, Tanner B, Schmid F, La Rocca V, Heinzer I, Bregenzer T. Impact of an infection control program on the prevalence of nosocomial infections at a tertiary care center in Switzerland. Infection Control & Hospital Epidemiology, 2008; 29(1):38-43.
- Ewans TM, Ortiz CR, LaForce FM. Prevention and control of nosocomial infection in the intensive care unit. In: Irwin RS, Cerra FB, Rippe JM, editors. Intensive Care Medicine. 4th ed. New York: Lippincot-Ravan; 1999; 074–80.
- Gaynes R, Edwards JR. Overview of nosocomial infections caused by gram-negative bacilli. Clin Infect Dis., 2005; 41:848–854.
- Olawale KO, Fadiora SO, Taiwo SS. Prevalence of Hospital-Acquired Enterococci Infections in Two Primary-Care Hospitals in Osogbo, Southwestern Nigeria. African Journal of Infectious Diseases, 2011; 5(2):40-46.
- Khan HA, Baig FK, Mehboob R. Nosocomial infections: Epidemiology, prevention, control and surveillance. Asian Pacific Journal of Tropical Biomedicine, 2017; 7(5):478-82.
- Chi SY, Kim TO, Park CW, Yu JY, Lee B, Lee HS, Kim YI, Lim SC, Kwon YS. Bacterial pathogens of ventilator associated pneumonia in a tertiary referral hospital. Tuberculosis and respiratory diseases, 2012; 73(1):32-7.
- Mehta Y, Gupta A, Todi S, Myatra SN, Samaddar DP, Patil V, Bhattacharya PK, Ramasubban S. Guidelines for prevention of hospital acquired infections. Indian journal of critical care medicine: peer-reviewed, official publication of Indian Society of Critical Care Medicine, 2014; 18(3):149.
- Abdellatif A, Bagian JP, Barajas ER, Cohen M, Cousins D, Denham CR, Essinger K, Gegelashvili G, Glenister H, Hoffman C, Horvath D. Improved Hand Hygiene to Prevent Health Care-Associated Infections: Patient Safety Solutions, Volume 1, Solution 9, May 2007. Joint Commission Journal on Quality and Patient Safety, 2007; 33(7):460-3.
- Lim SM, Webb SA. Nosocomial bacterial infections in Intensive Care Units. I: Organisms and mechanisms of antibiotic resistance. Anaesthesia, 2005; 60(9):887-902.
- Ducel JF. L. Nicolle Prevention of hospital-acquired infections WHO, Geneva (2002).
- Pfaller MA. Nosocomial candidiasis: emerging species, reservoirs, and modes of transmission. Clinical infectious diseases, 1996; 22(Supplement 2):S89-94.
© The Author(s) 2019. Open Access. This article is distributed under the terms of the Creative Commons Attribution 4.0 International License which permits unrestricted use, sharing, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.


