ISSN: 0973-7510
E-ISSN: 2581-690X
Hepatitis B is the most prevalent infection and a global concern that affects a large population. Healthcare workers (HCWs) are at higher risk of developing the disease, because of their regular contact with blood and body fluids. Objective of the study was to analyze all HCWs Knowledge, Attitude, and Practice (KAP) concerning hepatitis B infection and its vaccination, as well as the impact of educational training among them. A cross-sectional KAP study was done at a tertiary care hospital using a self structured questionnaire survey regarding hepatitis B infection and its vaccination among 156 HCWs. A short educational PowerPoint presentation (PPT) was given to them, followed by the same questionnaire survey. Pre and post-intervention data were collected to evaluate the effects of training on all HCWs. A Pre-assessment revealed that HCWs had inadequate KAP regarding Hepatitis B infection and vaccination. Ward attendants demonstrated the lowest grades in knowledge and practice and were identified as being at the highest risk. The instructional PPT intervention implemented in the study was proven to be highly effective. The results indicated a significant increase in knowledge and a favorable shift in the attitude towards hepatitis B infection and its vaccination among HCWs. Improvement in knowledge and attitude among all three types of HCW were extremely statistically significant after educational PPT presentation. Hence, this study recommends that increasing awareness of HBV infection and prevention through orientation and educational training, as well as routine tests and immunizations, will be beneficial.
KAP Study, Hepatitis B, Healthcare Workers, Vaccination
Hepatitis B is one of the major public health concerns around the world. The Hepatitis B virus (HBV) is the primary cause of this potentially fatal liver infectious disease. In an individual, it can manifest both in acute and chronic forms of liver disease.1,2 According to WHO, an estimated 8,20,000 deaths occurred worldwide from hepatitis B, mostly caused by cirrhosis and hepatocellular carcinoma (primary liver cancer) in the year 2019.1 In India, as per latest estimates, 40 million people are chronically infected with hepatitis B. The disease is mostly spread by contact with infected blood or other body fluids through the percutaneous or mucous membranes.3 In a healthcare setting, the risk of transmitting HBV infection (2-40%) following exposure to percutaneous injuries with infected blood is substantially higher than that of HCV (2.7-10%), HIV (0.3%) and other infections.4 Healthcare workers accounts for major-risk groups for this infection as they are exposed to a number of occupational hazards related to waste management, needle stick injuries, blood spillage, patient care and stress/violence in a healthcare setting.3,5 Hepatitis can be prevented by vaccines that are safe and effective. According to the Ministry of Health and Family Welfare, in India, vaccination coverage for Hepatitis -B birth dose was reported to be 76.36% as of December 2017 and there was no data available for routine Hepatitis B vaccination among health-care workers. A WHO study found that vaccination, diagnostic tests, medicines, and information campaigns might avert nearly 4.5 million premature deaths in low and middle-income countries by 2030. All WHO Member States have supported the WHO’s global hepatitis strategy, which targets to reduce new hepatitis infections by 90% and mortalities by 65% between 2016 and 2030.6,7 Education and raising awareness through frequent training programs on universal safety procedures such as use of gloves, PPE, mask, proper hand hygiene, safe injection practices and vaccination are the first and most important steps that must be followed in order to limit the risk of accidental transmission of Hepatitis B infection among HCWs.4,5 It is essential to review the knowledge, attitude and practices of healthcare professionals working in various healthcare settings globally to fill the information gap and henceforth work effectively and efficiently.
Aims
Objective of the study is to enhance healthcare personnel’s knowledge and improve their attitude and practices towards Hepatitis B infection and its vaccination and to check the impact of training provided to all HCWs.
Study Setting
The study was conducted at Nootan Medical College and Research Centre and Nootan General Hospital, Visnagar, Mehsana, Gujarat.
Study Design
Hospital based cross-sectional study to assess KAP of healthcare personnel.
Study population
Health care personnel (designated as staff nurses, laboratory technicians, and ward attendants). All the paramedical staff of the hospital was included, excluding doctors as they were fully vaccinated.
Sampling
The present study was conducted over a period of 3 months (June 2022 to August 2022). A total of 156 healthcare personnel were included in the study, which was divided into three groups. Group A: Staff Nurses, Group B: Laboratory technicians and Group C: Ward attendants (a hospital attendant who has general duties that do not involve the medical treatment of patients)
Data Collection
A self structured and self designed questionnaire with 35 questions- 15 for knowledge and 10 each for attitude and practice on hepatitis B infection and its vaccination was used to collect pre and post intervention data. The questionnaire was designed in both languages (English and Gujarati). Prior to data collection, investigators thoroughly briefed the participants about the goal of the study and the questionnaire. An intervention was made in the form of a short educational PPT prepared by investigators of the study regarding hepatitis B infection and its vaccination which was shown and briefed to all the participants. Post intervention data was collected after finishing the training session and it was done using the same questionnaire. Knowledge-based questions were graded by assigning a score of 1 to correct responses. For attitude questions, a favorable attitude received a score of 1. A score of 1 was assigned to satisfactory practices on the practice questions. Confidentiality of identity and data was maintained. The data was tabulated before being subjected to data analysis after data collection. Descriptive statistics i.e. percentage, differences in post and pre data, mean and standard deviation was used to describe studied variables. Pre and post questionnaire mean scores were compared to assess the impact of short educational PPT on HCW using paired t-test.
A total of (n=156) healthcare workers were involved in the study; of these, nurses made up the majority, accounting for 87 (55.7%) of the study participants, while lab technicians and ward attendants made up the remaining 35 (22.4%) and 34 (21.7%), respectively (Table 1).
Table (1):
Demographic traits of healthcare workers.
Demographic characteristics |
Numbers (%) |
|---|---|
Sex Male Female |
37(23.7) 119(76.2) |
Age Below 30 31- 50 Above 50 |
58(37.17) 82(52.56) 16(10.25) |
Job Category Nurses Laboratory technician Ward attendants |
87(55.7) 35(22.4) 34(21.7) |
Experience in healthcare < 5 years 6-10 years 11-15years 16-20 years >20 years |
41(26.2) 62(39.7) 35(22.4) 11(7.0) 07(4.4) |
Table (2):
Correct responses to knowledge questions about Hepatitis B infection and its vaccination.
| S. No. | Questions | Nursing Staff (87) | Lab technician (35) | Ward attendant (34) | Total Participants (n= 156) % | ||||
|---|---|---|---|---|---|---|---|---|---|
| Pre test | Post test | Pre test | Post test | Pre test | Post test | Pre test | Post test | ||
| 1 | Incubation period for Hepatitis B infection | 23 (26.4) | 78 (89.7) | 22 (62.86) | 23 (65.7) | 1 (2.94) | 8 (23.53) | 46 (29.48) | 109 (69.87) |
| 2 | Hepatitis B can be transmitted by EXCEPT | 20 (22.9) | 25 (28.8) | 17 (48.57) | 20 (57.1) | 5 (14.71) | 7 (20.59) | 42 (26.92) | 52 (33.33) |
| 3 | Highly infectious virus that can be transmitted through a drop of blood contaminated with infected patient | 18 (20.7) | 58 (66.7) | 14 (40) | 26 (74.3) | 1 (2.94) | 4 (11.76) | 33 (1.15) | 88 (56.41) |
| 4 | Which Body part is most affected by hepatitis B infection | 55 (63.2) | 81 (93.1) | 23 (65.7) | 29 (82.8) | 4 (11.76) | 17 (50) | 82 (52.56) | 127 (81.41) |
| 5 | Can Hepatitis B infection lead to Hepatic Cancer | 49 (56.3) | 69 (79.3) | 13 (37.1) | 25 (71.4) | 10 (29.41) | 23 (67.65) | 72 (46.15) | 117 (75) |
| 6 | First (early) investigation to carry out to know about Hep B infection | 66 (75.8) | 68 (78.16) | 28 (80) | 30 (85.7) | 10 (29.41) | 21 (61.76) | 104 (66.7) | 119 (76.3) |
| 7 | Recommended Hepatitis B vaccination schedule for adults | 49 (56.3) | 75 (86.2) | 19 (54.29) | 21 (60) | 17 (50) | 20 (58.82) | 85 (54.48) | 116 (74.35) |
| 8 | Route of administration of Hepatitis B vaccine | 56 (64.3) | 83 (95.4) | 20 (57.1) | 25 (71.4) | 8 (23.53) | 19 (55.88) | 84 (53.84) | 127 (81.41) |
| 9 | Can hepatitis B vaccine be given during pregnancy or lactation | 31 (39) | 49 (56.3) | 6 (17.1) | 11 (31.4) | 10 (29.41) | 18 (52.94) | 47 (30.12) | 78 (50) |
| 10 | Minimum protective titer required for HBs antibody | 39 (44.8) | 75 (86.2) | 14 (40) | 16 (45.71) | 15(44.12) | 17 (50) | 68 (43.58) | 108 (69.23) |
| 11 | If titer remains low after first series of vaccination, what is to be done | 14 (16) | 32 (36.7) | 12 (34.3) | 25 (71.43) | 12 (35.29) | 16 (47.06) | 38 (24.35) | 73 (46.79) |
| 12 | How long does protection from Hepatitis B vaccine last | 13 (15) | 15 (36.7) | 12 (34.29) | 22 (62.86) | 6 (17.65) | 9 (26.47) | 31 (19.87) | 46 (29.48) |
| 13 | Hepatitis B vaccine should be recommended in hospital settings to | 67 (77) | 74 (85) | 28 (80) | 31 (88.57) | 9 (26.47) | 15 (44.12) | 104 (66.66) | 120 (76.92) |
| 14 | Is it harmful to administer an extra dose(s) of Hepatitis B vaccine or repeat the entire vaccine series if documentation of vaccination history is unavailable | 30 (34.4) | 35 (40.2) | 14 (40) | 30 (85.7) | 13 (38.24) | 17 (50) | 57 (36.53) | 82 (52.56) |
| 15 | If a person has documentation of partial vaccination (1 or 2 doses), what is to be done | 46 (52.8) | 72 (82.7) | 20 (57.14) | 21 (60) | 17 (50) | 18 (52.94) | 83 (53.2) | 111 (71.15) |
Table 2 Illustrates the correct responses given by all the three groups of HCWs to knowledge based questions about Hepatitis B infection and its vaccination before and after receiving educational video training. Highest score of 104 (66.67%) obtained by HCWs in questions related to awareness about early investigation to carry out for Hepatitis B Infection (ques 6) and Hep B vaccination should be recommended in hospital settings (ques13). Poor scores were obtained on questions about highly infectious virus that can be transmitted through a drop of blood (ques 3) as well as how long the protection from Hep B vaccine lasts (ques12) was found in 33 participants (21.15%) and 31 participants (19.9%) respectively. Scores were improved to 119 (76.3%) and 120 (76.9%) for ques 6 and 13 whereas for ques 3 and ques 12 it was improved to 88(56.4%) and 46(29.4%) after post educational video intervention.
Table (3):
Total number of pre and post test scores with differences for knowledge based questions among each group of HCW.
Profession of healthcare workers (n=156) |
Pre test score (%) |
Post test score (%) |
Difference in score (%) |
|---|---|---|---|
Nursing staff (87) |
576 (44.13) |
889 (68.12) |
308 (23.9) |
Lab technician (35) |
262 (49.9) |
355 (67.61) |
93 (17.71) |
Ward Attendant (34) |
138 (27.05) |
229 (44.9) |
91 (17.8) |
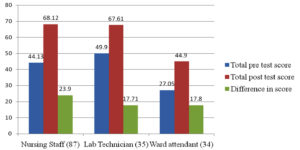
Table 3 shows the total number of pre and post test scores obtained separately by all the three groups of healthcare workers, with differences in scores indicating the impact of training. The percentage is calculated by dividing the total marks obtained by each category of HCW in the pre or post test by the total number of knowledge based questions (i.e.15), multiplied by the number of individual HCWs. According to the above table, there was a positive effect of training among nursing staff 308 (23.6%) as compared to lab technician 93 (17.71%) and ward attendants 91 (17.84%) (Figure 1).
Figure 1. Impact of training among all healthcare workers about knowledge on Hepatitis B infection and its vaccination
Table (4):
Favorable response to questions about attitude towards Hepatitis B infection and its vaccination.
| S. No. |
Questions | Nursing Staff (87) | Lab technician (35) | Ward attendants (34) | Total (%) | ||||
|---|---|---|---|---|---|---|---|---|---|
| Pre test |
Post test |
Pre test |
Post test |
Pre test |
Post test |
Pre test |
Post test |
||
| 1 | Do you have fear that you can get Hepatitis B infection? Yes No |
37(42.52) 50(57.47) |
21(24.13) 66(75.86) |
24(68.5) 11(31.4) |
15(42.9) 20(57.1) |
18(52.9) 16(47.1) |
7 (20.6) 27(79.4) |
79(50.6) 77(49.4) |
43(27.6) 113(72.4) |
| 2 | If Yes, Then Why? Get in contact with patients Exposure to needle stick injury Not fully vaccinated Contact with blood/ body fluids | 6(6.89) 13(14.94) 15(17.24) 3(3.44) |
5 (5.74) 8 (9.19) 6 (6.89) 2(2.29) |
2(5.71) 16(45.7) 4(11.42) 2(5.71) |
– 6(17.1) 6(17.1) 3(8.57) |
10(29.4) 4(11.76) 1(2.94) 3(8.82) |
1(2.94) 3(8.82) – 3(8.82) |
18(11.5) 33(21.2) 20(12.8) 8(5.12) |
6(3.84) 17(11) 12(7.7) 8(5.12) |
| 3 | If No, Then Why? Fully vaccinated Using of proper universal precautions Don’t know the consequences of Hepatitis B infection Aware about such type of infections | 10(11.49) 17(19.54) 9(10.34) 14(16.09) |
14(16.09) 12(13.79) 3(3.44) 37(42.52) |
4(11.42) 2(5.71) – 5(14.28) |
3(8.57) 1(2.85) 1(2.85) 15(42.9) |
4(11.76) 5(14.7) 1(2.94) 6(17.64) |
9(26.47) 6(17.64) – 12(35.3) |
18(11.5) 24(15.4) 10(6.41) 25(16) |
26(16.7) 19(12.2) 4(2.56) 64(41.1) |
| 4 | If you feel Loss of appetite, nausea, vomiting what will you do? Take old traditional remedies Immediately go to the physician Wait and go to physician after severity of the symptoms Test for Hepatitis B infection |
1(1.14) 51(58.62) 13(14.94) 22(25.28) |
– 66(75.86) 9(10.34) 12(13.79) |
3(8.57) 24(68.5) 3(8.57) 5(14.28) |
– 28(80) 1(2.85) 6(17.14) |
5(14.7) 16(47.1) 7(20.6) 6(17.6) |
2(5.88) 23(67.6) 5(14.7) 4(11.76) |
9(5.76) 91(58.3) 23(14.7) 33(21.2) |
2(1.3) 117(75) 15(9.6) 22(14) |
| 5 | If you are exposed with Hepatitis B positive blood, what will you prefer for immediate protection? Single dose of Hepatitis B vaccine Complete dose of Hepatitis B vaccine Passive immunization by HBIg Wait till clinical symptoms develop |
13(14.94) 45(51.72) 24(27.58) 5(5.74) |
6(6.89) 31(35.63) 49(56.32) 1(1.14) |
4(11.42) 23(65.7) 7(20) 1(2.85) |
2(5.7) 12(34.3) 21(60) – |
6(17.6) 14(41.2) 9(26.47) 5(14.7) |
4(11.76) 6(17.64) 24(70.6) – |
23(14.7) 82(52.6) 40(25.6) 11(7.05) |
12(7.7) 49(31.4) 94(60.3) 1(0.6) |
| 6 | If there is an interruption between Hepatitis B vaccination doses, what will you prefer? Will go for complete vaccination Second series of vaccination Ignore Don’t Know |
45(51.72) 25(28.73) 4(4.59) 13(14.94) |
63(72.4) 15(17.2) 1(1.14) 8(9.19) |
18(51.4) 9(25.71) 2(5.71) 6(17.14) |
31(88.6) 3(8.57) – 1(2.85) |
12(35.3) 6(17.6) 5914.7) 11(32.4) |
18(52.9) 12(35.3) 2(5.88) 2(5.88) |
75(48.1) 40(25.6) 11 (7.1) 30(19.2) |
112(72) 30(19.2) 3(1.9) 11(7.1) |
| 7 | Is it necessary to check antibody titer after getting Hepatitis B vaccine? Agree/ Disagree/ Don’t know |
63(72.41) 13(14.94) 11(12.64) |
82(94.2) 4(4.59) 1(1.14) |
27(77.1) 5(14.28) 3(8.57) |
29(82.9) 4(11.42) 2(5.7) |
12(35.3) 4(11.76) 18(52.9) |
31(91.1) 2(5.88) 1(2.94) |
102(65) 22(14.1) 32(20.5) |
142(91) 10(6.4) 4(2.56) |
| 8 | How will you react if your antibody titer is not up to the desired level? Shock Fear Surprise No effect |
11(12.64) 37(42.52) 8(9.19) 31(35.63) |
10(11.5) 20(23) 6(6.89) 51(58.6) |
15(42.9) 6(17.14) 5(14.28) 9(25.71) |
6(17.14) 8(22.86) 1(2.85) 20(57.1) |
7(20.6) 6(17.6) 9(26.47) 12(35.3) |
5(14.7) 4(11.76) 7(20.6) 18(52.9) |
33(21.2) 49(31.4) 22(14.1) 52(33.4) |
21(13.5) 22(14.1) 14(8.9) 89 (57) |
| 9 | Whom will you inform immediately after getting exposed to needle stick injury? Colleague Friends Infection Control officer Family |
2(2.29) 11(12.64) 69(79.31) 5(5.74) |
4(4.59) 1(1.14) 74(85.1) 8(9.19) |
4(11.42) 5(14.28) 24(68.5) 2(5.71) |
2(5.7) 1(2.85) 31(88.5) 1(2.85) |
8(22.9) 7(20.6) 10(29.4) 9(26.47) |
3(8.82) 1(2.94) 28(82.4) 2(5.88) |
14(8.97) 23(14.7) 103(66) 16(10.3) |
9(5.76) 3(1.92) 133(85) 11(7.1) |
| 10 | Would you like to share Razors, blade/ toothbrush with your family member? Yes No |
27(31.03) 60(68.96) |
10(11.5) 77(88.5) |
5(14.3) 30(85.7) |
2(5.7) 33(94.3) |
7(20.6) 27(79.4) |
5(14.7) 29(85.3) |
39(25) 117(75) |
17(11) 139(89) |
Table 4 Illustrates the favorable responses from all HCWs to questions about attitude towards Hep B infection and its vaccine. 117(75%) of the participants (n=156) have a positive attitude toward avoiding sharing their personal use items like razors, toothbrush with their family members(ques 10) and 102(65.4%) participants agreed that they should monitor the antibody titre level after getting vaccinated (ques7). There were 77(49.4%) study participants who had fear of getting Hep B infection (ques1). After the video intervention, their attitudes had changed to 139(89%) for ques10 and 142(91%) for ques7, although ques 1 on fear of Hep B infection had experienced a significant change in attitude, going from 77(49.4%) to 113(72.4%).
Table (5):
Total number of favorable responses on the pre and post tests and their difference in score related to attitude based questions on Hepatitis B infection and its vaccination.
Profession of healthcare Workers (n=156) |
Pre Favorable Response (%) |
Post Favorable Response (%) |
Difference in score (%) |
|---|---|---|---|
Nursing staff (87) |
407 (51.97) |
565 (72.15) |
158 (20.17) |
Lab technician (35) |
155 (49.20) |
228 (72.38) |
73 (23.17) |
Ward Attendant (34) |
120 (39.21) |
210 (68.62) |
90 (29.41) |
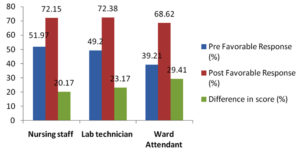
Table 5 describes the total number of favorable responses (ideal correct answers) given by each HCW towards the attitude based question of Hepatitis B infection and its vaccination before and after video intervention along with their differences. The impact of attitude towards this infection was highest among ward attendants 90(29.41%), followed by lab technicians 73(23.17%) and nursing staff 158(20.17%) (Figure 2).
Figure 2. Impact of training of all healthcare workers on their attitude toward Hepatitis B infection and its vaccination
Table (6):
Number of satisfactory responses to questions about practice toward Hepatitis B infection and its vaccination.
| S.no. |
Questions | Nursing Staff(87) | Lab technician(35) | Ward attendant(34) | Total % |
|---|---|---|---|---|---|
| Pre test | Pre test | Pre test | Pre test | ||
| 1 | How do you respond to Hepatitis B infected patients in a hospital setting? Treat patients with universal precaution Refer the patient Neglect the patient Not willing to treat the patient |
68(78.16) 7(8.04) 11(12.64) 1(1.14) |
14(40) 19(54.28) – 2(5.71) |
10(29.41) 13(38.23) 6(17.64) 5(14.7) |
92(58.97) 39(25) 17(10.89) 8(5.12) |
| 2 | Have you taken the Hepatitis B vaccination? Yes No |
63(72.41) 24(27.58) |
21(60) 14(40) |
19(55.88) 15(44.11) |
103(66.02) 53(33.97) |
| 3 | If Yes, how many Doses? 1 2 3 Do not remember |
6(6.89) 19(21.83) 22(25.28) 16(18.39) |
1(2.8) 9(25.71) 11(31.42) – |
4(11.76) 3(8.82) 11(32.35) 1(2.94) |
11(7.05) 31(19.87) 44(28.20) 17(10.89) |
| 4 | Did you ever tested for Hepatitis antibody titer? Yes No Don’t Know |
45(51.72) 36(41.37) 6(6.89) |
18(51.42) 13(37.14) 4(11.42) |
4(11.76) 17(50) 13(38.23) |
67(42.94) 66(42.30) 23(14.74) |
| 5 | Have you been exposed to Needle stick injury till today? Yes No |
29(33.34) 58(66.67) |
8(22.85) 27(77.14) |
19(55.88) 15(44.11) |
56(35.89) 100(64.10) |
| 6 | If yes, how many times you have been exposed to needle stick injury in last 12 months? 1 2 3 Multiple times |
15(17.24) |
3(8.57) |
5(14.70) |
23(14.74) |
| 7 | If yes, what immediate action you have taken after seeing blood coming out of your finger? Squeeze the finger Wash your finger under running water Put finger in the mouth Put cloth on the finger |
5(5.74) |
1(2.85) |
3(8.8) |
09(5.76) |
| 8 | If you had a needle stick injury to whom you have informed first? Colleague Infection control officer Took treatment by yourself Ignore |
4(4.59) 66(75.86) 16(18.39) 1(1.14) |
3(8.57) 24(68.57) 6(17.14) 2(5.7) |
11(32.35) 13(38.23) 2(5.88) 8(23.52) |
18(11.53) 103(66.02) 24(15.38) 11(7.05) |
| 9 | Are you recapping the needles after use? Yes No |
5(5.74) 82(94.25) |
7(20) 28(80) |
12(35.29) 22(64.70) |
24(15.38) 132(84.61) |
| 10 | How do you discard the needle after use? Red bag Blue cardboard box White puncture proof container Yellow bag |
5(5.74) 5(5.74) 74(85.05) 3(85.05) |
3(8.57) 1(2.85) 30(85.71) 1(2.85) |
6(17.64) 8(23.52) 19(55.88) 1(2.94) |
14(8.97) 14(8.97) 123(78.84) 05(3.20) |
| 11 | What are you doing for blood spill management in practice? Use 1% Sodium hypochlorite Dry/Wet mopping on floor Ignore Don’t know |
64(73.56) 13(14.94) 2(2.29) 8(9.19) |
28(80) – – 7(20) |
22(64.70) 3(8.82) 7(20.58) 2(5.88) |
114(73.07) 16(10.25) 09(5.76) 17(10.89) |
| 12 | Are you sharing your Razor/ Blade with family members? Yes No |
1(16.09) 73(83.09) |
8(22.85) 27(77.14) |
6(17.64) 28(82.35) |
28(17.94) 128(82.05) |
| 13 | Have you participated in any training or continuing education related to any infection? Yes No |
55(63.21) 32(36.78) |
21(60) 14(40) |
22(64.70) 12(35.29) |
98(62.82) 58(37.17) |
Table 6 denotes the number of satisfactory responses of the practices followed by all the HCWs regarding Hepatitis B infection and its vaccination. Good practices were mostly followed by all HCWs for not sharing their personal use items to their family members (ques 9) was found in 128(82.05%) and recapping the needles after use (ques 6) was found in 132 (84.61%). Also, discarding the needle after every use (ques7) was found in 123(78.9%) study participants. Being a healthcare professional, a shocking response was noted in only 53(33.97%) participants for not taking vaccination for Hepatitis B infection.
Table (7):
Illustrates the total number of satisfactory responses of the practices followed by each healthcare worker regarding Hepatitis B infection and its vaccination.
Profession of healthcare workers |
Satisfactory Responses (%) |
|---|---|
Nursing Staff (87) |
670 (70) |
Lab Technician (35) |
249 (64.67) |
Ward Attendant (34) |
185 (49.46) |
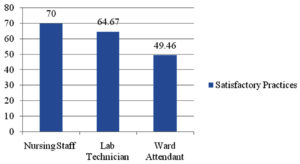
Table 7 and Figure 3 describes the satisfactory responses of the practices followed by all the healthcare workers regarding hepatitis B infection and its vaccination working in our hospital.
Figure 3. Impact of training among all healthcare workers about practices regarding Hepatitis B infection and its vaccination
We found that KAP mean scores of nursing staff was highest as compared to Lab technicians and ward attendants as shown in Table 8.
Table (8):
Mean score of pre and post intervention responses on knowledge, attitude and practice regarding hepatitis B infection and its vaccination.
| Groups |
Knowledge (Mean±SD) |
Attitude (Mean±SD) |
Practice (Mean±SD) | ||||
|---|---|---|---|---|---|---|---|
| Pre intervention | Post intervention | P- value* | Pre intervention | Post intervention | P- value* | Pre intervention | |
|
Nursing Staff |
38.40±18.53 | 59.27±22.37 | =0.0001 | 45.22±18.65 | 62.78±14.63 | <0.0001 | 57.5±19.53 |
|
Lab- technician |
17.47±6.19 | 23.67±5.50 | =0.0003 | 17.22±9.43 | 25.33±6.38 | =0.0005 | 21.25±7.64 |
|
Ward attendants |
9.20±5.14 | 15.27±5.61 | <0.0001 | 13.38±6.02 | 23.33±6.24 | =0.0011 | 16.42±6.73 |
* Paired t-test
Healthcare workers are at risk of exposure, possible transmission and infection of hepatitis B because the majority of them are in constant contact with patients or infective material from patients. Knowledge, Attitude and Practice of employees at the workplace towards these infections are key to preventing one from getting nosocomial diseases.2 Most of the earlier KAP studies conducted in India were observational studies. In our present study, we implemented an intervention in the form of educational video demonstration to all the participants and measured its impact on knowledge and attitude scores.8 Our study includes 156 total healthcare workers, out of which 87(55.76%) were Nursing staff, 35(22.43%) were lab technicians and 34(21.79%) were ward attendants. Among them, female candidates were 119(76.30%) and the male candidates were only 37(23.70%). Similarly in the study of Gurubacharya DL9 female candidates 59(84%) were more than the male candidates 11(1%). Most of the candidates were aged between 31-50 years 82(52.56%) followed by below 30 years of age 58(37.17%) and more than 50 years of age 16(10.25%). Among total (n=156) candidates, 62(39.7%) had experience of 6-10 years and only 7(4.4%) had an experience of more than 20 years (Table 1). Likewise in the study of Shah PD they showed 29(38.6%) candidates had experience of 3-10 years and 19 (25.3%) had experience of more than 20 years.
The findings of the present study discovered some interesting facts regarding KAP of HCWs concerning some important aspects of hepatitis B infection and its vaccination. Results showed that among all HCW, nursing staff and lab technician had good knowledge as compared to ward attendants, whereas ward attendants showed unfavorable attitudes and unsatisfactory practices towards hepatitis B infection and its vaccination which is quite a matter of concern. Level of knowledge about hepatitis B infection and its vaccination is diverse among the different categories of healthcare personnel which might be due to differences in their level and type of education.
Out of 156 HCWs, almost 109(69.87%) candidates knew about the incubation period of Hepatitis B infection, whereas only 63(84%) of participants were having knowledge about incubation period in the study of Shah et al.,8 52(33.33%) and 88(56.41%) HCWs were aware about the mode of transmission and the transmission through the drop of blood respectively similarly in the study of Aniaku, et al.,7 79.6% students knew about the transmission of Hepatitis B infection. Approximately 82(52.56%) and 72(46.15%) HCWs were knew about the fact that the liver is the most affected organ by Hepatitis B virus and lead to cancer but after educational training it was increased up to 127(81.41%) and 117(75%) respectively. Bharti et al.,10 and Shrestha et al.,11 showed 96.7% and 43.6% knowledge regarding the same. About the investigation of the Hepatitis B, nearly 119(76.28%) candidates knew, whereas in the study of Abdela et al.,12 showed relatively lower proportion of the students (52.4 %).knew that HBV has treatments.
When asked about prevention, 116(74.35%) and 127(81.41%) candidates were aware about the schedule of vaccination doses and the route of administration. Similarly, Bhattarai et al.2 and Shrestha et al.11 observed 316 (77.4%) and 145 (80.1%) participants knew about the recommended complete doses schedule. Knowledge about the minimum protective titer of HBs antibody must be > 10 IU/ml and the protection of the vaccine could last for at least 20 years was observed in 108(69.23%) and 46(29.48%) HCWs but in the study of Bhattarai S. et al.2 showed only 122 (29.9%) and 160 (39.2%) candidates knew about the same. Overall ward attendants showed poor knowledge about Hepatitis B infection and its vaccination but all participants were provided adequate knowledge on hepatitis B and its vaccination through educational video and the results shows that training is necessary in all levels of health care workers.
Among all the categories of HCWs, nursing staff had the highest favorable attitude towards hepatitis B infection and its vaccination i.e 407(51.97%) which was increased up to 565(72.15%) after the educational training. Majority of the candidates 113 (72.43%) had no fear about getting Hepatitis B infection because they are aware about such infections, whereas the results in the study of Abdela et al.12 are in concordance with our result where 223 (90.7%) candidates are not scared of Hepatitis B infection. The study done by Shah et al.,8 89.3% consulted a doctor after exposure to infected blood which is higher than our study where 94(60.25%) believed that they should take the vaccine after exposure to the blood and body fluids. In the study of Shrestha et al.,11 50.8% (n = 92) agreed that hepatitis B vaccination is safe and effective, while in our study 112 (71.79%) would go for the full vaccination if there is any interruption in the vaccination doses. Most of the candidates believed 142(91.02%) that it is necessary to check anti-HBsAg antibodies titer after getting vaccine which is higher than the study done by Gurubacharya et al.,9 where only 6 workers (14%) had been tested for Anti-HBs. The Centre for Disease Control (CDC) recommendation is to test for antibodies after completion of three injections of HBV vaccine, and if negative, give a second three-dose vaccine and test again for anti-HBsAg antibodies. If there is no antibody response, no further vaccination is recommended.9 Shockingly 22 (14.10%) candidates feared that the Anti-HBs titer would not rise to the desired level whereas 89 (57.05%) had no effect. Regarding immediate information to be given after exposure to NSI, Alsabaani et al.,3 showed 59.4% or 30.9% agreed that all sharp injuries at work should be reported immediately whereas in our study 133(85.23%) candidates agreed about the same.
Practices concerning prevention of Hepatitis B infection were satisfactory in which nursing staff showed highest safe practices that is 670 (70%). When asked HCWs about response towards Hepatitis B infected patients, 92 (58.97%) candidates were treating them with universal precautions however, 39 (25%) would like to refer the patient Shrestha et al.11 showed that 6.6% (n = 12) strongly agreed on feeling uncomfortable while sitting with a Hepatitis B positive person and 18.8% (n = 34) strongly disagreed. In our study, 44(28.20%) HCWs were fully vaccinated (three doses) while 42(26.92%) HCWs were partially vaccinated. Around 67(42.94%) HCWs checked anti-HBsAg titre. However in the study of Rathi, et al.,13 observed only 13 (8%) had received a completed course of hepatitis B vaccination while 30 (18.7%) had history of inability to complete the three doses of hepatitis B vaccination The reasons for not getting vaccinated might be lack of interest, fear of injection or adverse reaction or planning to get immunized later.
Health care workers should be aware about exposure to the blood and the body fluids as they are highly prone to getting infections. In our study 56(35.89%) HCWs had exposed to NSI and mostly 23(14.74%) had exposed once in a year and after exposing to the NSI 103(66.02%) believed that it is necessary to report the incident to the Infection control officer but Gurubacharya et al.,9 showed higher results than our study where 52 subjects (74%) out of 70 had a history of needle-stick injury and out of those, 27(52%) had 1 -2 pricks per year. This somehow reflects their lack of responsibility towards themselves. Most of the needle stick injuries might be caused while recapping of needle 24(15.38%). Sharma et al14 also showed 33.5% had NSI but 26.3% had reported the incident and they were caused while doing IM/IV procedures (36.1%) and recapping of needles (32.8%). Reason behind NSI could be due to rush and uncooperative behavior of the patients. Shockingly 38(24.35%) HCWs were washing their fingers after exposure to the NSI. 123(78.84%) candidates were disposing needles into the white puncture proof container which is in concordant with the study of Sharma et al.14 where 84.8% candidates disposing needles correctly. Approximately 114(73.07%) HCWs were practicing correct method of preparation of 1% sodium hypochlorite from the 5% strength for the blood spillage management likewise in the study of Mehta et al.,15 where 40.6% (n=28) nurses and 42.46% (n=31) doctors were doing correct Blood spillage management. Most of our HCWs 128(82.05%) were not sharing a blade/razor with the family members while in study of Shrestha et al.,11 the majority 129(71.3%) ask for a new blade while cutting or shaving hair. Nearly 98(62.82%) participated previously in the health campaign or training. Results are quite high compared to the study done by Shah PD et al.,8 where only 49.3% candidates participated previously in training, so it is very evident that training programmes should be conducted at regular intervals in healthcare settings.
This type of HCW assessment and training has not been conducted in our healthcare setting; therefore this study and training were helpful for all HCWs as there was an improvement found in KAP with reference to hepatitis B infection and its vaccination.
This study emphasizes the lack of understanding regarding HBV infection and its vaccination. Therefore, it is strongly advised that healthcare facilities should change their training programmes to give HCWs, the knowledge and skills they need. In order to attain universal coverage, healthcare facilities should develop measures to provide HBV testing and immunization to all medical personnel.
Based on the findings of our study, HCWs had inadequate knowledge and attitude about some crucial aspects of hepatitis B infection and its vaccination. However, after the educational intervention there was a significant impact observed among HCW’s on the subject. The most devastating situation was of the ward attendants who had the lowest grades in terms of knowledge and practices and were consequently most at risk of contracting Hepatitis B infection. Because they come into contact with the sample and patients directly, HCWs should be encouraged to regularly assess their anti-HBs antibody titre at regular intervals. This led to the conclusion that spreading sufficient knowledge about HBV infection and prevention through orientation and sensitization programmes, educational training, and promotions will be helpful. It will be beneficial to foster a positive mindset among healthcare professionals, which will result in good practices. In addition, it should be made mandatory for all healthcare workers to undergo routine screenings and receive the appropriate vaccinations.
Strength and Limitation
Gaining knowledge is frequently the first step in changing a desirable behavior. A sufficient amount of education and sensitization will likely lower the rate of new infections among HCWs as well as the stigma associated with the illness. The drawbacks in our study are that we have not observed anti-HBs status of HCWs for HBV vaccination to check their vaccination status.
ACKNOWLEDGMENTS
The authors would like to thank all the nursing staff, technicians, and ward attendants for their participation and support throughout the study.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORS’ CONTRIBUTION
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
FUNDING
None.
DATA AVAILABILITY
All datasets generated or analyzed during this study are included in the manuscript.
ETHICS STATEMENT
This study was approved by Institutional Ethics Committee, Nootan Medical College and Research Centre, Visnagar, Gujarat, India, with reference number IEC/NMCRC/46/2022.
- World Health Organization (WHO) news-room/fact-sheets/detail/hepatitis-b, Accessed 24 June, 2022. https://www.who.int.
- Bhattarai S. Knowledge, Attitude and Practice of Hepatitis B Vaccination among Health Care Workers at Manipal Teaching Hospital. Kathmandu Univ Med J. 2020;72(4):361-366.
Crossref - Alsabaani A, Alqahtani NSS, Alqahtani SSS, ia. Incidence, Knowledge, Attitude and Practice Toward Needle Stick Injury Among Health Care Workers in Abha City, Saudi Arabia. Front. Public Health. 2022;10:771190.
Crossref - Abuduxike G, Acar Vaizoglu S, Asut O, Cali S. An Assessment of the Knowledge, Attitude, and Practice Toward Standard Precautions Among Health Workers From a Hospital in Northern Cyprus. Saf Health Work. 2021;12(1):66-73.
Crossref - World Health Organization (WHO)/health-topics/ hepatitis. Accessed 24 June, 2022 https://www.who.int/india.
- World Health Organization (WHO). Hepatitis. Accessed June 24, 2022. Available at: https://www.who.int/health-topics/hepatitis#tab=tab_1.
- Aniaku JK, Amedonu EK, Fusheini A. Assessment of Knowledge, Attitude and Vaccination Status of Hepatitis B among Nursing Training Students in Ho, Ghana. Annals of Global Health. 2019; 85(1):18:1-9.
Crossref - Shah PD, Mehta TK, Patil LV. Interventional Knowledge, Attitude and Practice Study Regarding Hepatitis B Virus Infection and its Vaccination Using Educational Video Among Health Care Workers. Natl J Community Med. 2019;10(3):130-134.
- Gurubacharya DL, KC Mathura, Karki DB.Knowledge, attitude and practices among health care workers on needle-stick injuries. Kathmandu University Medical Journal. 2003;1(2):91-94.
- Koria B, Lala MK. A study of knowledge, attitude and practice of hepatitis-B infection among the laboratory technicians in the civil hospital, Ahmedabad, Gujarat. Healthline. 2012;3(1):63-65.
- Shrestha DB, Khadka M, Khadka M, Subedi P, Pokharel S, Thapa BB. Hepatitis B vaccination status and knowledge, attitude, and practice regarding Hepatitis B among preclinical medical students of a medical college in Nepal. PLoS ONE. 2020;15(11):e0242658.
Crossref - Abdela A, Woldu B, Haile K, Mathewos B, Deressa T. Assessment of knowledge, attitudes and practices toward prevention of hepatitis B virus infection among students of Medicine and Health Sciences in Northwest Ethiopia. BMC Res Notes. 2016;9(1):41.
Crossref - Rathi A, Kumar V, Majhi J, Jain S, Lal P, Singh S. Assessment of knowledge, attitude, and practices toward prevention of hepatitis B infection among medical students in a high-risk setting of a newly established medical institution. J Lab Physicians 2018;10:374-937.
Crossref - Sharma A, Singh C, Solanki S, Satishkumar, Mehrishi P, Faujdar SS. Prevalence and Knowledge of Needle Stick Injury among the Health Care Workers in a Tertiary Care Hospital Solan H.P, India. Int J Curr Microbiol App Sci. 2017;6(8):2486-2492.
Crossref - Mehta TK, Shah PD, Tiwari KD. A Knowledge, Attitude and Practice Study of Biomedical Waste Management and Bio-safety among Healthcare Workers in a Tertiary Care Government Hospital in Western India. Natl J Community Med. 2018;9(5):327-333.
© The Author(s) 2023. Open Access. This article is distributed under the terms of the Creative Commons Attribution 4.0 International License which permits unrestricted use, sharing, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.