ISSN: 0973-7510
E-ISSN: 2581-690X
One of the biggest risks to public health is tuberculosis (TB), an infectious disease caused by the Mycobacterium tuberculosis bacteria. As one of the most communicable diseases in the present day, tuberculosis has historically claimed more lives than any other infectious disease, leading to high rates of morbidity and mortality. Despite being present, it is still disregarded by clinicians as a cause of extrapulmonary tuberculosis. This case report focuses on an atypical presentation of an extrapulmonary tuberculosis (EPTB) infection in the form of a soft tissue mass presenting as a chest wall abscess in an immunocompetent person. This case was identified and managed appropriately. This atypical case presentation without lung involvement indicates that a complete case analysis is necessary. In this case, diagnosis was established using microbiological methods, molecular, imaging, and histopathological diagnosis. However, this example clarifies an essential lesson that the shift is beginning from pulmonary to extrapulmonary tuberculosis cases.
Atypical Case Report, Extrapulmonary Tuberculosis, Immunocompetent, Paucibacillary, Soft Tissue Tuberculosis
According to the World Health Organisation (WHO), coronavirus disease in 2019 was the leading infectious disease cause of death globally, followed by tuberculosis (TB). From 1.5 million in 2020 to 1.4 million in 2019, it led to an estimated 10.6 million new patients and 1.6 million deaths worldwide in 2021. According to these figures, decades of global progress in reducing TB mortality has been disrupted by the COVID-19 pandemic, and the total number of TB-related deaths in 2020 has returned to the level seen in 2017.1 Tuberculosis is considered as chronic granulomatous disease primarily caused by inhalation of airborne droplets contaminated with M. tuberculosis.2 TB is a treatable illness that can manifest in either a pulmonary or extrapulmonary manner. Because extrapulmonary tuberculosis is still difficult to diagnose because of its atypical presentation, medical practitioners must be aware of it in order to recognise it, treat it, and reduce needless mortality.3 In this case report patient was having soft tissue tuberculosis of chest wall without involvement of bony structure.
Case Scenario
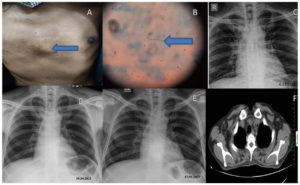
A 44-year old male, farmer by occupation presented in general surgery out-patient department in tertiary care hospital with 6 month history of swelling on anterior chest wall (Figure 1A) along with symptoms of fatigue. It had progressively increased in size without any pain and erythema. History of weight loss was present. There was no fever, shortness of breath, cough, night sweats. Patient was given an antibiotic during the initial visit to reduce swelling without further investigation, but after the treatment failed, surgeons sent the pus they had drained for regular bacterial processing and histopathology. All frank pus samples are routinely processed for Ziehl-Neelsen staining (ZN stain) and Potassium hydroxide microscopic examination (KOH) for AFB and fungal organisms, respectively, and this sample was no exception. After regular bacteriological processing, the sample was sterile. Acid-fast bacilli were found in the sample (Figure 1B). For Mycobacteria Growth Indicator Tube culture (MGIT), Cartridge based nucleic acid amplification test (CBNAAT), and Lowenstein-Jensen medium (LJ) culture, additional processing was carried out. Rifampicin-sensitive MTB bacilli were found by CBNAAT. After 14 days, MGIT culture detected TB bacilli, from that capillia test was showed positive and LJ culture showed rough, buff and tough colonies after 5 weeks of incubation. On histopathology findings were suggestive of caseous tuberculous necrosis. Simultaneously patient was also further investigated which stated that patient was immunocompetent but haemoglobin was decreased on haemogram. Sputum sample was investigated for acid fast bacilli but found to be negative. X-ray lung of previous 2 years and recent showed no obvious abnormality related to tuberculosis (Figure 1C, 1D, 1E). Contrast-enhanced computed tomography (CECT) (Figure 1F) of lung was also done to confirm further spread and lung involvement. CECT of lung revealed no lung involvement without any old tubercular lesion or any bone erosion. Well defined hypodense collections in anterior chest wall at the level of body on sternum and right 2nd and 3rd intercostal space without any bony erosion. Patient was immediately contacted and treatment started.
Figure 1. Showing Clinical, Microbiological and Radiological images (A). Midsternal abscess (Blue arrow showing abscess); (B). Ziehl Neelson Stain (Blue arrow showing Acid Fast Bacilli); (C, D, E). Showing postero-anterior view of Chest X-ray showing no obvious abnormality; (F). Contrast-enhanced computed tomography (CECT) of lung showing no lung or bone involvement
Tuberculosis is of two types pulmonary and extrapulmonary. Extrapulmonary TB involve lymph node, meninges, kidneys, bone, skin and the oral cavity.2 Extrapulmonary TB is difficult to diagnose because of its paucibacillary nature and atypical clinical manifestation. It presents with clinical symptoms and signs such as non-healing abscess, pus, bone pain, infertility, lymph node swelling, meningitis, osteomyelitis which resembles other microbiological infectious conditions which may be confusing for physician sometimes. So many of times, antibiotic treatment is given to patients which leads to antibiotic resistance. Out of all cases of EPTB, lymph node TB accounts for 30-40%, pleural TB for 20%, abdominal TB for about 12%, genitourinary TB for 20%, osteoarticular TB for 11%, meningitis TB for 5-10%, and cutaneous & musculoskeletal TB for 1-5% of cases. The least prevalent kind of tuberculosis is musculoskeletal TB. Due to its late and unique presentation, it is challenging to diagnose.4
There is also no specific guideline for treatment of extrapulmonary tuberculosis. Most of the physician follow TB treatment similar to treatment of pulmonary TB. So delay in diagnosis and treatment can result in increased mortality and morbidity.5,6 Non-specific treatment, incomplete treatment gives rise to XDR and MDR TB. One of the most pressing and challenging issues facing global TB control is the growth of drug-resistant TB. Patients with multidrug-resistant (MDR) TB, which is caused by strains of the disease that are resistant to isoniazid and rifampicin, are essentially incurable with first-line treatment.7 MDR-TB are resistant to any fluoroquinolones and at least one of the second-line injectable medications (capreomycin, kanamycin, and amikacin) are referred to as extensively drug-resistant (XDR) TB. Weak medical systems, transmission in communities and facilities, and amplification of resistance patterns due to improper treatment are the primary drivers of the spread of resistant TB. Risk factors for MDR-TB are no response to a first-line DOTS regimen (WHO Category I or II), HIV coinfection, areas with high prevalence of MDR-TB, defaulter patient, close contact with MDR-TB patients.7
Our patient had a slow-growing, asymptomatic abscess when they first arrived. He never had TB before or exposed to any known TB positive patient. First time the clinician assumed it was a bacteriological infection due to its unusual presentation.
Positive M. tuberculosis bacilli identification on culture and histology are a prerequisite for a conclusive diagnosis of EPTB. In this case report we couldn’t provide histopathological data photos as well as treatment and follow up of details patient. This is limitation of our study.
The hematogenous and lymphatic spread of the M. tuberculosis bacterium results in extrapulmonary tuberculosis (EPTB). The development of active TB infection and the reactivation of latent TB are both predisposed by the alteration in immune state followed by granuloma formation. In an immunocompetent person who has never been exposed to tuberculosis, the emergence of sensitization to mycobacterial antigen is necessary for tuberculosis pathogenesis. Caseating granulomas and cavitation are two pathologic symptoms of tuberculosis that are brought on by hypersensitivity reactions.8 Chest wall tuberculosis typically presents as a cold abscess, with mildly elevated inflammatory markers and little constitutional symptoms. It is advised that all patients have their pulmonary involvement assessed due to the 10-15% concurrent lung infection rate with EPTB.9 Imaging aids in evaluating the severity and concurrent infections. In our case, a CT scan was required to rule out osteomyelitis and was helpful in identifying any lung diseases. Saldana et al reported chest wall tuberculosis without pulmonary involvement in three pediatric patients. They were immunocompetent.10 Heravati et al. reported TB case where 15 year old boy who has had previous history of tuberculosis presented with chest wall tuberculosis.11 In our case patient was immunocompetent and presented with soft tissue swelling without any lung involvement which was atypical presentation as this clinically can be presented in case of bacterial, fungal, cancer lesion so we have to consider all of them including tuberculosis infection.
TB can manifest in the body at several locations. According to the World Health Organisation, 16% of TB cases are caused by EPTB. 10-35% of these are musculoskeletal, and just 1% of them are limited to the chest wall. As patient was from rural area and had gone to multiple clinicians but was misdiagnosed. He was willing to start treatment and get cured after counseling. To prevent the disease’s further spread, morbidity, and death, we must now raise physician awareness of extrapulmonary tuberculosis infection and encourage them to begin treatment as soon as possible.
ACKNOWLEDGMENTS
The authors acknowledges everyone who assisted in this case study.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORS’ CONTRIBUTION
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
FUNDING
None.
DATA AVAILABILITY
All datasets generated or analyzed during this study are included in the manuscript.
ETHICS STATEMENT
This study was approved by the Institutional Ethics Committee, Mahatma Gandhi Institute of Medical Sciences, Wardha, Maharashtra, India, vide reference number MGIMS/lEC/MICR/101/2019.
INFORMED CONSENT
Written informed consent was obtained from the participant before enrolling in the study.
- World Health Organization. WHO Global Task Force on TB Impact Measurement: report of a subgroup meeting on methods used by WHO to estimate TB disease burden, 11-12 May 2022, Geneva, Switzerland. World Health Organization; 2022.
- Sriram S, Hasan S, Saeed S, Ahmad SA, Panda S. Primary tuberculosis of buccal and labial mucosa: literature review and a rare case report of a public health menace. Case Rep Dent. 2023;2023(1):6543595.
Crossref - Saxena S, Hariharan D. Extrapulmonary tuberculosis presentation in the form of a chest wall abscess with no pulmonary involvement in the UK: a case report. J Surg Case Rep. 2022;2022(9):rjac421.
Crossref - Gopalaswamy R, Dusthackeer VNA, Kannayan S, Subbian S. Extrapulmonary tuberculosis—an update on the diagnosis, treatment and drug resistance. J Respir. 2021;1(2):141-64.
Crossref - Jorstad MD, Aẞmus J, Marijani M, Sviland L, Mustafa T. Diagnostic delay in extrapulmonary tuberculosis impact onpatient morbidity: A study from Zanzibar. PloS one. 2018;13(9):e0203593.
Crossref - Wolde HF, Clements AC, Alene KA. Health system and environmental factors affecting global progress towards achieving End TB targets between 2015 and 2020. J Glob Health. 2025;15:04004.
Crossref - Seung KJ, Keshavjee S, Rich ML. Multidrug-resistant tuberculosis and extensively drug-resistant tuberculosis. Cold Spring Harb Perspect Med. 2015;5(9):a017863.
Crossref - Ramirez-Lapausa M, Menendez-Saldana A, Noguerado-Asensio A. Extrapulmonary tuberculosis.Rev Esp Sanid Penit. 2015;17(1):3-11.
Crossref - Lee JY. Diagnosis and treatment of extrapulmonary tuberculosis. Tuberc Respir Dis. 2015;78(2):47.
Crossref - SaldaNa NG, Parra MM, de la Garza EA, et al. Case report: chest wall tuberculosis without pulmonary involvement in three pediatric immunocompetent patients. Am J Trop Med Hyg. 2019;101(5):1073.
Crossref - Herawati A, Nugraha J, Winarno DJS, Rizki M. Chest wall tumor tuberculosis in Indonesian adolescent: A rare case. Int J Surg Case Rep. 2022;98:107587.
Crossref
© The Author(s) 2025. Open Access. This article is distributed under the terms of the Creative Commons Attribution 4.0 International License which permits unrestricted use, sharing, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.