ISSN: 0973-7510
E-ISSN: 2581-690X
Healthcare-associated infections (HAI) are associated with increased morbidity, mortality and associated financial burden. Nosocomial blood stream infections in NICU remain a serious hazard. This was a prospective study done from January to December 2016. 1064 neonates admitted to NICU during this period were enrolled in the study. Active surveillance in NICU and laboratory based surveillance in Department of Microbiology was carried out to find cases of nosocomial blood stream infections. Each case was line listed and followed with calculation of attack and incidence rates. Out of the total 1064 new admissions between January and December 2016, 30 cases of hospital acquired infections were identified based on risk factors, clinical and laboratory data. Out of these twenty cases were hospital acquired blood stream infections. Average attack rates of HAI and hospital acquired blood stream infection were 2.76% and 1.93% respectively. Incidence of HAI/1000 patient days was 5.57 with BSI rate of 12.74. / 1000 catheter days. The most common organisms isolated from positive blood cultures were Staphylococcus aureus (32.4%), Acinetobacter spp. (24%) and E. coli (11.3%). BSI in NICU remains a serious hazard and remains grossly underreported. Infection control policies and surveillance methodologies need to be strengthened to curb BSI.
HAI, Nosocomial Infections, BSI, NICU, Infection Control.
Healthcare-associated infections (HAI) are associated with increased morbidity, mortality, and associated financial burden.1 HAI in the neonatal intensive care units (NICUs) are affected by many factors like infection control practices, endemic microbial flora, invasive procedures, parenteral nutrition and antibiotic stewardship policies.2 Environmental factors, hospital policies and unit epidemiology also play an important role.2 Neonatal infections remains a huge challenge for pediatricians, infection control teams, quality managers and administrators. Nosocomial infections increase the cost of neonatal intensive care, prolong hospital stay and are responsible for almost half of the deaths that occur beyond two weeks of age.3 Emergence of resistant strains are another unwanted consequence of antibiotic selection pressure. Blood stream infection (BSI) is considered a serious hazard because of their frequency (59%) amongst HAI and potential life- threatening consequences.4
Surveillance is a basic and effective strategy to gauge and contain HAI. Monitoring neonatal infections is increasingly regarded as an important parameter for safety and quality of healthcare delivery.5 For many countries including India, the magnitude of HAI’s are not exactly known or is grossly underestimated.6 This is mainly because HAI’s diagnosis is complex and surveillance activities to guide interventions require expertise and resources. Thus, this study was designed to monitor the trends of nosocomial blood stream infections in NICU.
Study design and patient population
This was a prospective study over a period of one year from January to December 2016. 1064 neonates admitted to NICU during this period were enrolled in the study. Active surveillance in NICU and laboratory based surveillance in Department of Microbiology was carried out to find cases of nosocomial blood stream infections. Blood stream infection was monitored prospectively by the attending pediatric staff, infection control team and clinical microbiologist. Demographic, clinical and microbiological data were prospectively collected and recorded on a performa. Each case was line listed and followed with calculations of attack and incidence rates as per the following definitions.
Attack rate: (Number of new nosocomial infections acquired in a period/number of patients observed in the same period) X 100
Incidence rate: (Number of new nosocomial infections acquired in a period/total patient days for the same period) X 1000
Definitions and criteria
Hospital acquired blood stream infections
Neonates who had no infection and / or were not in the incubation period at presentation and who developed infection more than 72 hours after hospitalization. Blood stream infections were identified on basis of clinical signs of sepsis and / or positive blood cultures. All blood cultures were processed by the bacteriology laboratory in department of microbiology. BSI was defined as isolation of at least one positive peripheral blood culture, whereas for cases of coagulate negative staphylococci infection two positive blood cultures were required.
Laboratory tests
Blood culture bottles were incubated for 7 days at 37°C and sub cultured at 24 hours, 72 hours and 7 days of incubation into sheep blood agar and MacConkey agar. Cultures were incubated at 37 °C for 24-48 hours. Isolates of bacteria were identified by conventional biochemical and serological methods .The antibiotic susceptibility for isolated pathogens was performed on Muller Hinton agar (HiMedia) by Kirby- Bauer disk diffusion method and interpreted according to the Clinical Laboratory Standards Institute breakpoint values.
Out of the total 1064 new admissions between January and December 2016, thirty cases of hospital acquired infections were identified based on risk factors, clinical and laboratory data. Out of these twenty cases were hospital acquired blood stream infections. Average attack rates of HAI and hospital acquired blood stream infection were 2.76% and 1.93% respectively. Incidence of HAI/1000 patient days was 5.57 with BSI rate of 12.74. / 1000 catheter days. The most common organisms isolated from blood cultures were Staphylococcus aureus (32.4%), Acinetobacter spp. (24%) and E. coli (11.3%). In S. aureus maximum resistance was seen with penicillin (74%). Acinetobacter spp. was resistant to Amoxicillin clavulanic acid (83%), Amikacin (66%) and Ceftriaxone (77%). In E. coli 88% resistance was seen to Amoxicillin clavulanic acid, Ciprofloxacin (79%) and Ceftriaxone (77%).
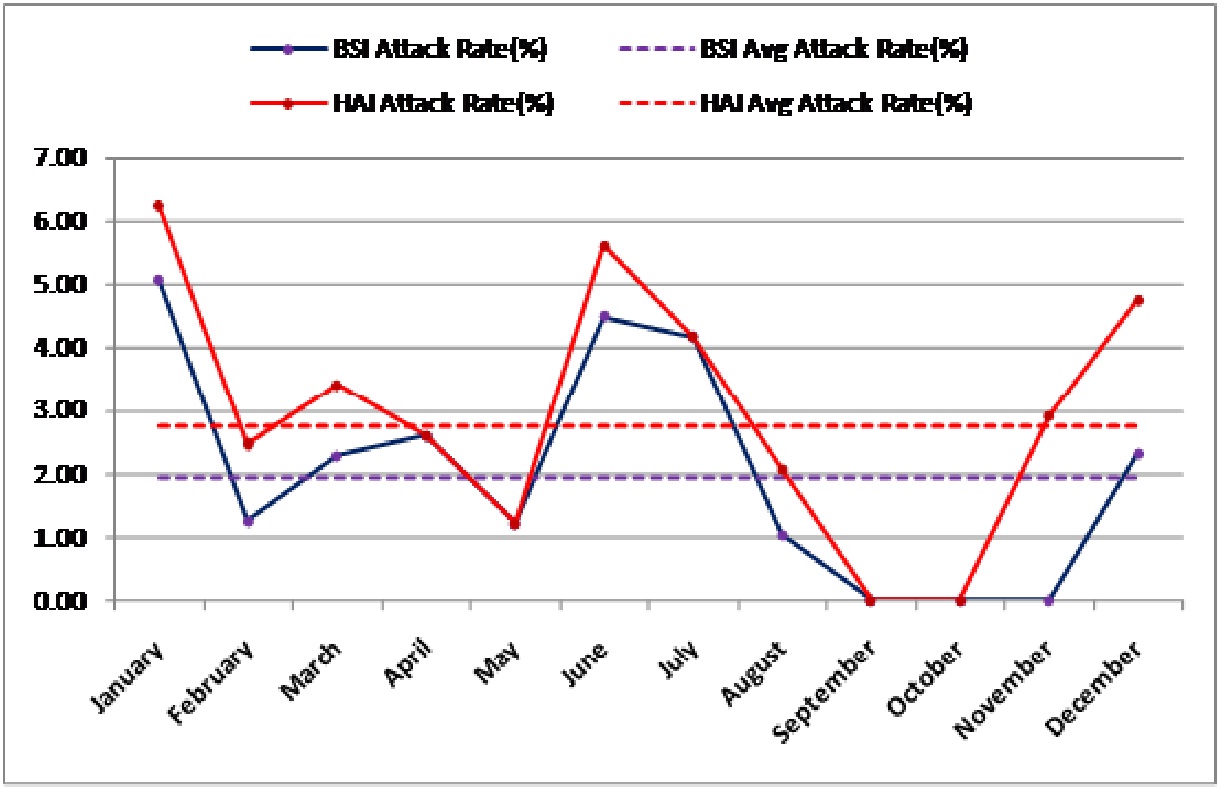
Fig. 1: Attack rates of BSI and HAI
Table (1):
HAI surveillance rates in NICU.
Month |
No of new admissions |
No. of BSI |
No of HAI |
Catheter days |
Patient Days |
BSI Attack Rate (%) |
HAI Attack Rate (%) |
BSI/1000 catheter days |
Incident of HAI/1000 Pt Days |
|---|---|---|---|---|---|---|---|---|---|
January |
79 |
4 |
5 |
133 |
596 |
5.06 |
6.23 |
30.07 |
8.38 |
February |
81 |
1 |
2 |
136 |
579 |
1.23 |
2.46 |
7.35 |
3.45 |
March |
88 |
2 |
3 |
169 |
601 |
2.27 |
3.40 |
11.8 |
4.99 |
April |
77 |
2 |
2 |
122 |
502 |
2.59 |
2.59 |
16.3 |
3.98 |
May |
98 |
1 |
1 |
120 |
584 |
1.20 |
1.20 |
8.33 |
1.71 |
June |
89 |
4 |
5 |
167 |
612 |
4.49 |
5.61 |
23.9 |
8.16 |
July |
72 |
3 |
3 |
134 |
633 |
4.16 |
4.16 |
22.38 |
4.71 |
August |
97 |
1 |
2 |
129 |
622 |
1.03 |
2.06 |
22.38 |
4.71 |
September |
104 |
0 |
0 |
133 |
644 |
0 |
0 |
0 |
0 |
October |
92 |
0 |
0 |
164 |
– |
0 |
0 |
0 |
0 |
November |
103 |
0 |
3 |
178 |
630 |
0 |
2.91 |
0 |
9.52 |
December |
84 |
2 |
4 |
148 |
531 |
2.3 |
4.76 |
13.5 |
7.51 |
Total |
1064 |
20 |
30 |
1729 |
6534 |
1.93 |
2.76 |
12.74 |
5.57 |
BSI attack rate was seen above the average rate in the months of January, March, April, June, July and December. However, the difference from the average was not found to be significant for any of these months. Incidence of BSI was seen above the average rate in the months of January, April, June, July and December. However, the difference from the average rate was not found to be significant. Incidence of HAI was seen above the average rate in the months of January, June, November and December. However, the difference from the average was not found to be significant.
Neonatal infections are an important reason for infant mortality and morbidity worldwide. In our study, incidence of HAI/1000 patient days was 5.57 which were consistent with the results of other studies. As per WHO prevalence study amongst 55 hospitals in four WHO Regions (Europe, Eastern Mediterranean, South- East Asia and western Pacific) 8.7% HAI rates were reported.7 A meta analysis by Neeraj et al estimated that different HAI rates were found varying from 1.4% upto 30% in numerous studies done across the globe.6 In another study, by Bolat et al the incidence of HAI was 10.3% per 1000 patient days.8 According to a survey to determine the point prevalence of HAI in 29 high- risk nurseries in 1999 by the US Pediatric Prevention Network, 11. 4% neonates had an active nosocomial infection on the day of the survey.9 Bloodstream and lower respiratory tract infection were the most frequent infections in the study.9
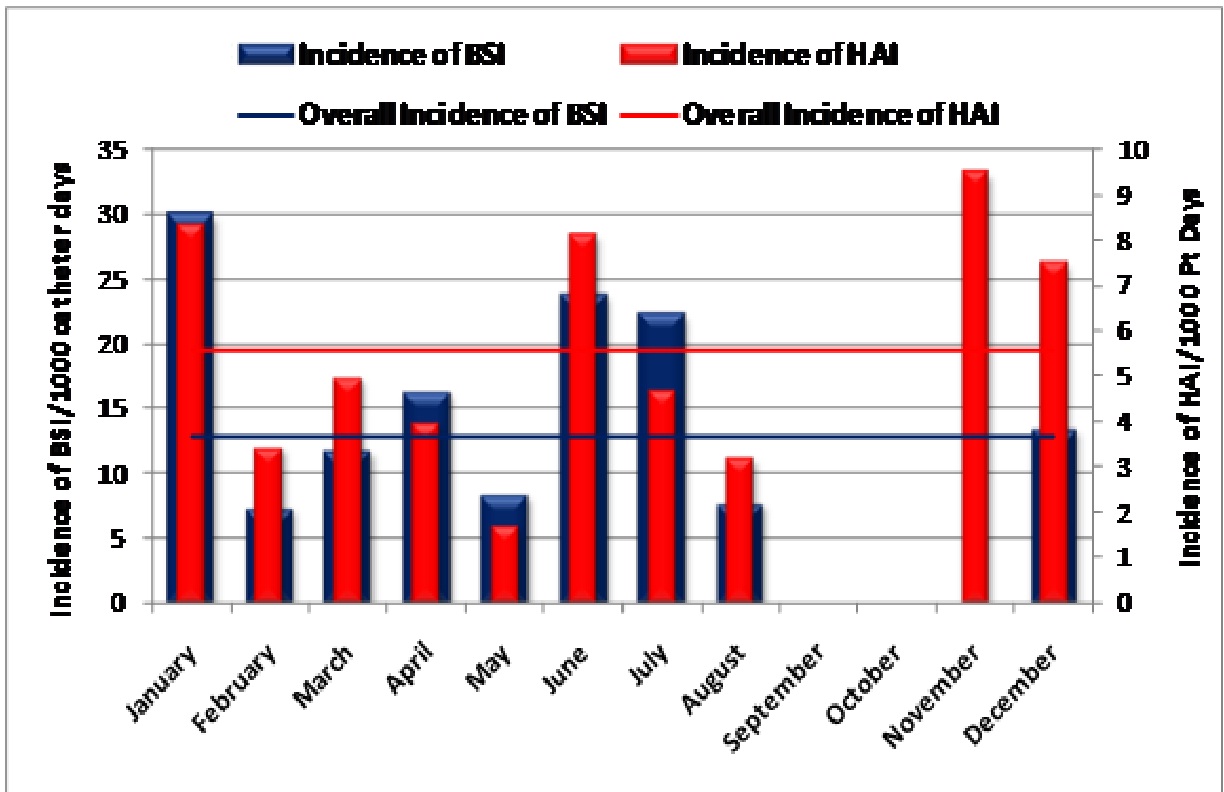 Fig. 2: Incidence rates of BSI and HAI
Fig. 2: Incidence rates of BSI and HAITable (2):
Attack rates of BSI and HAI in NICU.
| Month | No. New Admissions | No. of HAI | No. of BSI | BSI Attack Rate | HAI Attack Rate | ||
|---|---|---|---|---|---|---|---|
| % | p-value | % | p-value | ||||
| January | 79 | 5 | 4 | 5.06 | 0.204 | 6.23 | 0.202 |
| February | 81 | 2 | 1 | 1.23 | 0.568 | 2.46 | 0.862 |
| March | 88 | 3 | 2 | 2.27 | 0.830 | 3.4 | 0.740 |
| April | 77 | 2 | 2 | 2.59 | 0.715 | 2.59 | 0.925 |
| May | 98 | 1 | 1 | 1.2 | 0.507 | 1.2 | 0.156 |
| June | 89 | 5 | 4 | 4.49 | 0.244 | 5.61 | 0.243 |
| July | 72 | 3 | 3 | 4.16 | 0.343 | 4.16 | 0.552 |
| August | 97 | 2 | 1 | 1.03 | 0.380 | 2.06 | 0.627 |
| September | 104 | 0 | 0 | 0 | NA | 0 | NA |
| October | 92 | 0 | 0 | 0 | NA | 0 | NA |
| November | 103 | 3 | 0 | 0 | NA | 2.91 | 0.928 |
| December | 84 | 4 | 2 | 2.30 | 0.821 | 4.76 | 0.389 |
| Total | 1064 | 30 | 20 | 1.93 | – | 2.76 | – |
In our study out of the total thirty HAI episodes reported over a period of one year, 20 (66.6%) were nosocomial blood stream infections. Our findings are supported by observation in another study where BSIs (59.1%) were the most common HAI in this age group.10 On the contrary, in a recent study from Egypt, pneumonia was the most frequently occurring infection (11.3%) followed by blood stream infection (8.8%) in NICU.11According to recent studies primary bloodstream infection represents about 15% of all nosocomial infections and affects approximately 1% of all hospitalized patients.12 BSI increases the mortality rate and prolongs intensive care unit (NICU) and hospital length of stay with added financial burden.13 Our study observed 12.74% BSI/1000 catheter days. Our findings are supported by two studies where BSI incidence rates were 8.5 per 1000 discharges to 18 per 1000 patient days.14, 15
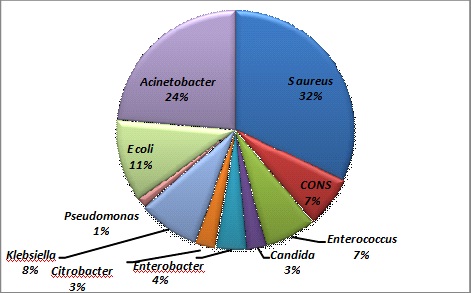
Fig. 3: Prevalence of isolates in blood cultures
Table (3):
Incidence rates of BSI and HAI.
Month |
No. of new admissions |
No. of HAI |
No. of BSI |
Catheter Days |
Patient Days |
Incidence of BSI/1000 catheter days |
p-value* of BSI Incidence Comparison from Overall |
Incidence of HAI/1000 Pt Days |
p-value* of HAI Incidence Comparison from Overall |
|---|---|---|---|---|---|---|---|---|---|
January |
79 |
5 |
4 |
133 |
596 |
30.07 |
0.367 |
8.38 |
0.784 |
February |
81 |
2 |
1 |
136 |
579 |
7.35 |
0.570 |
3.45 |
0.745 |
March |
88 |
3 |
2 |
169 |
601 |
11.8 |
0.935 |
4.99 |
0.938 |
April |
77 |
2 |
2 |
122 |
502 |
16.3 |
0.805 |
3.98 |
0.825 |
May |
98 |
1 |
1 |
120 |
584 |
8.33 |
0.631 |
1.71 |
0.355 |
June |
89 |
5 |
4 |
167 |
612 |
23.9 |
0.491 |
8.16 |
0.786 |
July |
72 |
3 |
3 |
134 |
633 |
22.38 |
0.580 |
4.73 |
0.917 |
August |
97 |
2 |
1 |
129 |
622 |
7.75 |
0.575 |
3.21 |
0.681 |
September |
104 |
0 |
0 |
133 |
644 |
0 |
NA |
0 |
NA |
October |
92 |
0 |
0 |
160 |
– |
0 |
NA |
0 |
NA |
November |
103 |
3 |
0 |
178 |
630 |
0 |
NA |
9.52 |
0.680 |
December |
84 |
4 |
2 |
148 |
531 |
13.5 |
0.952 |
7.53 |
0.835 |
Total |
1064 |
30 |
20 |
1729 |
6534 |
12.74 |
– |
5.57 |
– |
* p-values are calculated for comparison of incidence rate of particular month with the average using Gaussian (z) test.
Our study recorded average attack rates of hospital acquired infection and blood stream infection as 2.76% and 1.93% respectively. A similar study on 367 hospitalized patients, identified 29 patients with nosocomial BSI with attack rate of 7.9%.16
Our study observed that Staphylococcus aureus was the most frequently isolated organisms (32.4%) among the blood culture. Our findings were supported by another study where Staphylococcus aureus was the most frequent pathogen in culture positive BSI.17 On the contrary in another descriptive hospital based study carried out in the NICU of the Mansoura University Children’s Hospital, the investigators reported that Klebsiella spp. were the most frequently isolated organisms followed by E. coli.11 Gram- negative bacteria were the most common causative agents in hospital acquired bloodstream infection in the 1960s and 1970s.18 However, around the same time frame, gram-positive bacteria became more predominant, probably correlated with the greater use of prophylactic antibiotics for at risk patients with use of intravascular devices.18
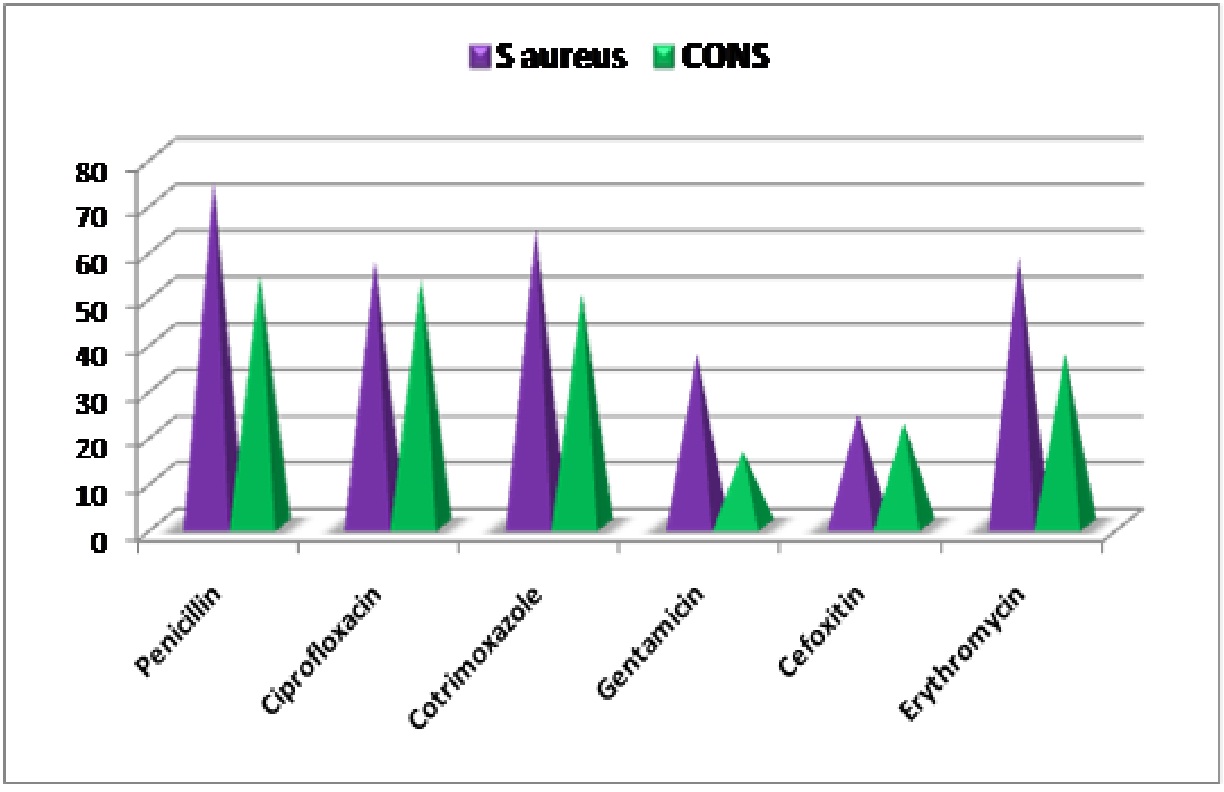 Fig. 4: Antimicrobial Susceptibility for gram positive cocci isolates
Fig. 4: Antimicrobial Susceptibility for gram positive cocci isolates
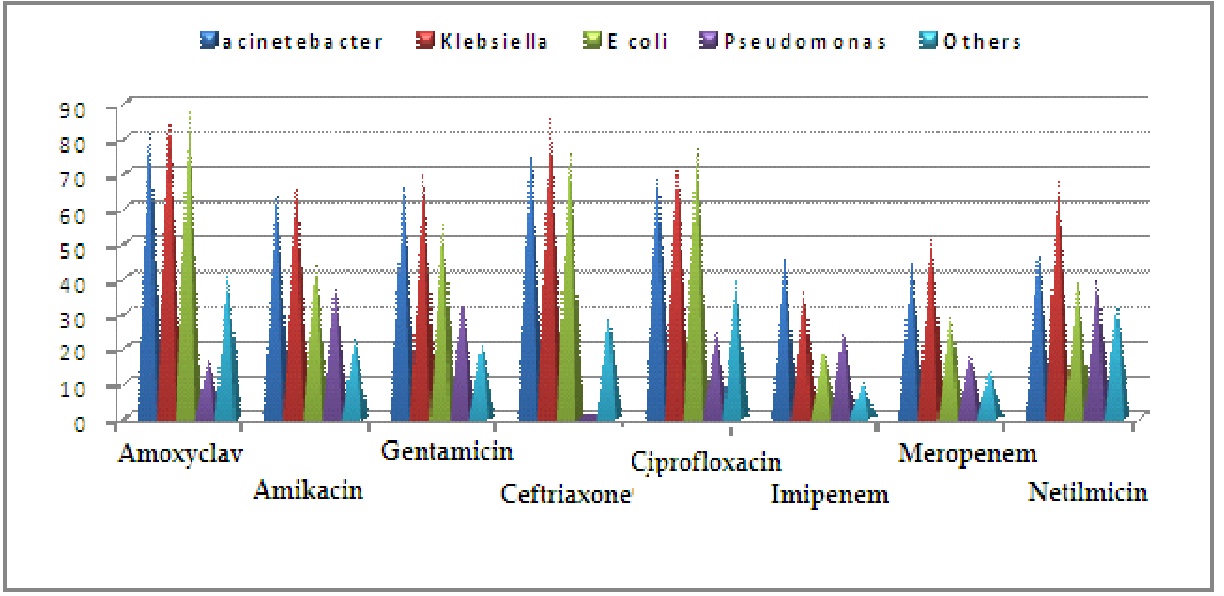 Fig. 5: Antimicrobial susceptibility for gram negative bacilli isolates
Fig. 5: Antimicrobial susceptibility for gram negative bacilli isolatesInfection control is an integral part of pediatric practice. Infection surveillance in nurseries and NICU should be conducted on a priority basis. The infection and the attack rates can be used as a benchmark to drive improvements in the quality and safety of care. Surveillance is also essential to decrease the mortality rate, economic burden and for rational antimicrobial prescription. Regular training programs on the standard precautions, hand hygiene, personal protective equipment, clinical sample collection and transport should be incorporated. Hand washing and regular use of alcohol based hand rub are the simplest and most effective methods of preventing transmission of infectious agents.19 Sterilization of resuscitation bags and masks, use of sterile suctioning techniques, and avoiding overcrowding are simple ways to prevent nosocomial infections in nurseries and NICUs.20 Careful preparation and storage of infant formulas, minimizing the attempts at venipuncture and, using single dose administration of medications such as albumin are measures to be undertaken to prevent nosocomial BSIs.21 Judicious insertion and maintenance of indwelling lines with minimization of the number of catheter days lowers the risk of device associated BSI.21
Limited information is available regarding epidemiology of health care associated infections and it seems that many HAIs are grossly under reported in many health care settings. BSI in NICU still remains a serious hazard and remains grossly underreported. Infection control practices and training program should focus on BSI prevention, recognition and reporting. Infection control policies and surveillance methodologies need to be strengthened. HAI reporting process should be revalidated.
- Revelas A. Healthcare-associated infections:A public health problem. Niger Med J. 2012; 53(2):59-64.
- Rania Mohammed Kishk, Mohamed Fouad Mandour. Pattern of Blood Stream infections within Neonatal Intensive Care Unit, Suez Canal University Hospital, Ismailia, Egypt. Int J Mocrobiol. 2014: 276-873.
- Akram Niknajad, Moteza Ghojazadeh. Factors Affecting the Neonatal Intensive care Unit Stay Duration in Very Low Birth Weight Premature Infants. J Caring Sci. 2012; 1(2):85-92.
- Anadel Rio, Carlos Cervera. Patients at Risk of Complications of Staphylococcus aureus Bloodstream Infection. Clinical Infectious Diseases. 2009; 48(4):246-253.
- Gray JW. Surveillance of Infection in neonatal intensive care units. Early Hum Dev. 2007; 83(3):157-63.
- Bedi Neeraj and Nasir Ahmad Ali. Health care associated (HAI’s) –a major patient safety issue. Ejpmr. 2016; 3(4):163-167.
- Prevention of hospital- acquired infections.A practical guide 2nd edition. WHO/CDS/CSR/EPH/2002.12.
- Faith bolat, Sinan uslu. Healthcare- associated infections in a neonatal intensive care unit in turkey. Indian Pediatrics. 2012;49: 947-8.
- Klara M Posfay- Barbe, Prof Danielle M Zerr. Infection control in pediatrics. 2008; 8(1):19-31.
- Tammy Bischoff, Hilmar Wisplingloff. Nosocomial Bloodstream infections in US Hospitals: Analysis of 24,179 cases from a prospective nationwide surveillance study. Clinical Infectious Diseases. 2016; 39(3):309-317.
- Abdel- Wahab F, Goneim M. Nosocomial infection surveillance in an Egyptian neonatal intensive care unit. J Hosp Infect. 2013; 83(3):196-9.
- Stephane Hugonnet, Hugo Sax. Nosocomial Bloodstream Infection and Clinical Sepsis. Emerge Infect Dis. 10(1):76-81.
- Vineet Chopra, Sarah L Krein. Prevention of Central Line- Associated Bloodstream Infections: Brief Update Review Evidence Reports/ Technology Assessments, No. 211. Rockville (MD): Agency for Healthcare Research and quality (US);2013 Mar.
- Abou Elella R, Najm HK, Balkhy H, Bullard L, Kabbani MS et al Impact of bloodstream infection on the outcome of children undergoing cardiac sugery. Pediatric cardiology. 2010; 31(4):483-9.
- Babay HA, Twum-Danso K, Kambal AM, Al-Otaibi FE. Bloodstream infections in Pediatric Patients, Saudi Med J. 2005; 26(10):1555-61.\
- Hilmar Wisplingloff, Walter Perbix, Harald Seifert. Risk Factors for Nosocomial Bloodstream Infections due to Acinetobacter baumannii: A Case-Control Study of Adult Burn Patients. Clinical Infectious Diseases 1999; 28:59–66.
- Vibhor Tak, Purva Mathur, Sanjeev Lalwani, Mahesh Chandra Misra. Staphylococcal Blood Stream Infections: Epidemiology, Resistance Pattern and Outcome at a Level 1 Indian Trauma Care Center. J Lab Physicians. 2013; 5(1): 46–50.
- Mariana V. Arnoni; Eitan N. Berezin; Marinês D.V. Martino. Risk factors for nosocomial bloodstream infection caused by multidrug resistant gram-negative bacilli in pediatrics. Braz J Infect Dis, 2007; 11(2).
- Purva Mathur. Hand hygiene: Back to the basics of infection control. Indian J Med Res. 2011; 134(5): 611–620.
- Emine Alp,Andreas Voss. Ventilator associated pneumonia and infection control. Ann Clin Microbiol Antimicrob. 2006; 5: 7.
-
Linda Tietjen Débora Bossemeyer Noel McIntosh. Infection Prevention Guidelines for Healthcare Facilities with Limited Resources.. www.jhpiego.org.
© The Author(s) 2017. Open Access. This article is distributed under the terms of the Creative Commons Attribution 4.0 International License which permits unrestricted use, sharing, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.