ISSN: 0973-7510
E-ISSN: 2581-690X
Newborns have the highest risk of death in the first 4 weeks of their life. Umbilical cord of a child is an important site for microorganism colonization and also forms a portal of entry for invasive pathogens. This study focuses on the bacterial colonization with 2 separate cord care regimens: dry cord and 4% chlorhexidine care group. This is a randomized control time-bound study conducted at a tertiary health care centre in Mangalore. A total of 144 newborns fulfilling the inclusion criteria were included and then divided randomly into two groups: dry cord care and 4% chlorhexidine. Two swabs were collected, baseline swab (swab 1) within 3 hours of birth and second swab (swab 2) at 120± 10 hours of birth and these samples were cultured for gram negative and positive organisms. Results were evaluvated with Chi-Square test. Out of 144 samples, in 115 showed no growth at the baseline and only 29 showed growth. In the dry cord care group, 38.9% showed growth of microorganism in comparison with chlorhexidine group which was 1.4% in swab 1 (baseline) and in swab 2, 87.5% in dry cord care group and 18.1% in chlrohexidine group in swab 2 respectively. It was observed that methicilin susceptible Staphylococcus aureus (MSSA) and methicillin resistant Staphylococcus aureus (MRSA) were the most common microorganisms isolated with others being Pseudomonas species, coagulase-negative Staphylococci (CoNS), Enterobacter species and Citrobacter species. Use of 4% chlorhexidine is effective in reducing colonization of bacteria and infection in comparison with dry cord care method. Therefore, decontamination of the umbilical cord with 4% of chlorhexidine should be recommended in a newborn child. However, both cord care methods did not lead to any infections.
4% Chlorhexidine, Cord Care, Colonization
The neonatal period is one of the most crucial periods for a new-borns survival. On an average 18 deaths per 1000 live births occur globally (2021) during this period.1 Infection is one of the chief cause.2 Among the numerous risk factors of new-born’s infections, the umbilical region is considered as an important site of microorganism colonization and point of entry for invasive pathogens.3
The infections of the umbilical stump can be localized or might rapidly progress to florid systemic sepsis,4 hence umbilical stump care has a very important role in hygienic neonatal practices and the prevention of sepsis in new-born.5-7 Cord care practices vary according to the region, culture, socioeconomic status, etc.8
Over the past few decades, chlorhexidine has been widely used for its broad-spectrum antiseptic properties.9 It is one of the most affordable and efficacious interventions in preventing infections and in improving neonatal survival in low-resource settings such as ours. So far, studies have shown chlorhexidine application has a lower infection among neonatal intensive care units,10 when WHO recommends keeping the cord clean and not to apply anything to it (dry cord care).11,12 Though there are studies regarding the application of CHX for umbilical cord care but not in Indian population and also culture of the microorganisms are not done till date to our knowledge.
Therefore, this study aimed to assess the bacterial decontamination on the umbilical cord with two methods- dry cord care method and application of 4% chlorhexidine.
This is a non randomized control time-bound sudy (September 2019 to September 2021) done at a Tertiary care centre, Government Lady Goschen Hospital, Mangalore, Dakshina Kannada District, Karnataka. Study included neonates born through a cesarean section of ≥ 34 weeks of gestation, hemodynamically stable and not requiring NICU. This study excluded, babies born to the mothers having HIV, hepatitis B, active tuberculosis, with suspected septicemia, fever with rash, features of urinary tract infection, prolonged rupture of membranes (>18 hours) and babies by mother’s side but on antibiotics.
Sample size was calculated using the formula:
n = (Z1-a/2) √2PQ + Z1-b √P1Q1 + P2Q2 / (P1 – P2)
Total of 144 newborns were included with 72 each in both arms of the study with convenient sampling. The study was initiated after seeking approval from the Institutional ethical committee (IEC KMC MLR 10-19/494), and CTRI registration (REG No: CTRI/2020/05/025266). Parents of the newborn fulfilling the inclusion criteria were approached and were briefed about the study objectives and a participant information sheet was provided explaining the most asked queries. Written consent was obtained from the parents agreeing to participate and was allocated into one of the groups by a single investigator. In dry cord care group, the cord was cleaned with sterile gauze to clean the blood stains after birth and dried and exposed to air and parents/ caregivers were advised to wipe with gauze after bath and to tie the diaper/cloth below the umbilical cord stump. In the intervention group, 4% chlorhexidine supplied in 10ml eyedropper bottles was applied one time daily until the cord separated. Sufficient quantity of chlorhexidine was applied by the principal investigator on day 1 and cord was left untouched for 3-5 minutes, mothers were taught to apply under supervision and were instructed to apply once per day. Mothers were taught to identify the signs and symptoms of infection of the umbilical stump. Under aseptic precautions, swabs for culture using sterile swabs were taken from the base of the umbilical stump. The first umbilical swab sample (swab 1) was taken within three hours of birth and the second umbilical swab (swab 2) at 120 ± 10 hours of birth and cultured from each of the participants. Swabs were transported to the laboratory at room temperature within 6 hours of collection. Culture media used for culture and sensitivity were Mac Conkey’s media for gram-negative organisms and Blood agar and Chocolate agar for gram-positive organisms. Culture reports were available after 48 hours and were identified based on their growth pattern. Standard laboratory techniques were used to identify Staphylococcus spp. isolated from solid-medium blood cultures. These techniques served as the gold standard by which the quick tests sensitivity and specificity were measured. The test was scored as positive if a clot formed. Tubes with a negative result were incubated overnight and read again the next day. Clinical examination for signs and symptoms of cord infection was done daily by an independent investigator who had no knowledge to which group the neonate belonged to. If signs of umbilical infections developed, parents were informed to come to the hospital for follow-up and treatment.
The collected data was coded onto excel sheet and analysed using the IBM SPSS (Statistical Package for Social Sciences) for Windows version 25.0, Armonk, NY:IBM Corp. For the continuous variables were expressed as mean and standard deviation, categorical variables were expressed as frequency and percentage. Two groups were compared using chi-square test. P-value of <0.05 was considered statistically significant.
It was noticed that out of 144, 79.9% (115) of the baseline swab (swab 1) showed no growth and the rest 21.1% (29) had growth. It was observed that methicilin susceptible Staphylococcus aureus (MSSA) (10.4%) and methicillin resistant Staphylococcus aureus (MRSA) (5.6%) were the most common microorganisms isolated with others being Pseudomonas species (2.1%), coagulase-negative Staphylococci (CoNS), Enterobacter species and Citrobacter species.
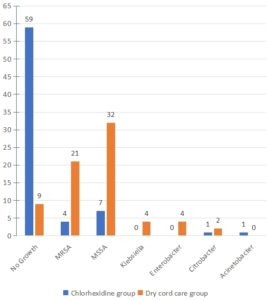
In the dry cord care group, 28(38.9%) and 63(87.5%) had growth of microorganisms in baseline swabs (swab 1) and swab 2, respectively. MRSA and MSSA were the most common organisms isolated. MSSA accounted for 19.4% and 44.4% in swab 1 and 2, respectively. MRSA growth was 11.1% and 29.2% in swab 1 and 2, respectively. This was statistically significant with a P value (Table).
In chlorhexidine group, 1.4% and 18.1% of swab 1 and swab 2 respectively had growth. MSSA was the only microorganism isolated from swab 1. While MSSA (9.7% cases), MRSA (5.6% cases), Citrobacter species and Acinetobacter were isolated from swab 2 of the chlorhexidine group. This was statistically significant with P value < 0.001. On day 5 swab (swab 2) of both the group, 18.1% and 87.5% grew microorganisms in the chlorhexidine group and dry cord care group respectively. There was statistically significant growth in swab 2 of the dry cord care group in comparison with swab 2 of the chlorhexidine group (Table).
Table :
Growth pattern in dry cord care and 4% chlorhexidine group
| Dry Cord Care | 4% Chlorhexidine | |||||
|---|---|---|---|---|---|---|
| Growth Pattern | SWAB 1 | SWAB 2 | P Value | SWAB 1 | SWAB 2 | P Value |
| n (%) | n(%) | <0.001 | n (%) | n(%) | <0.001 | |
| No Growth | 44 (61.1%) | 9 (12.5%) | 71 (98.6%) | 59 (81.9%) | ||
| Methicillin-resistant Staphylococcus aureus (MRSA) | 8 (11.1%) | 21 (29.2%) | – | 4(5.6%) | ||
| Methicillin-susceptible Staphylococcus aureus (MSSA) | 14 (19.4%) | 32 (44.4%) | 1(1.4%) | 7(9.7%) | ||
| Coagulase-negative Staphylococci (CoNS) | 1 (1.4%) | – | – | – | ||
| Klebsiella species | – | 4 (5.6%) | – | – | ||
| Enterobacter species | 1 (1.4%) | 4 (5.6%) | – | – | ||
| Citrobacter species | 1 (1.4%) | 2 (2.8%) | – | 1(1.4%) | ||
| Pseudomonas species | 3 (4.2%) | – | – | – | ||
| Acinetobacter species | – | – | – | 1(1.4%) | ||
| Total | 72 (100) | 72 (100) | 72(100%) | 72(100 %) | ||
Organisms isolated in swab 2 of the chlorhexidine group were MSSA (9.72%), MRSA (5.55%), Citrobacter species and Acinetobacter species. In swab 2 of the dry cord care group MSSA (44.44%), MRSA (29.16%), Klebsiella species, Enterobacter species and Citrobacter species were isolated (Figure).
Though there were growth of microorganisms (colonisation) in both the groups, no case of infection was observed in the study.
This study focuses on the bacterial decontamination on the umbilical cord with two methods that is the dry cord care regimen versus the topical application of 4% chlorhexidine. In this study, newborns satisfying the inclusion criteria were recruited. Gender of the babies in both the study group was nearly equal with majority of them being term newborns with weight between 2500 to 3500 grams. Chlorhexidine is active in many forms, but 4% is the recommended dosage for neonatal cord care (chlorhexidine di-gluconate 7.1% in aqueous solution or gel); therefore, 4% is applied in our study.13,14
Some of the studies conducted in Africa found that, 4% chlorhexidine did not reduce neonatal mortality,15 but studies from South Asian countries found its effect towards positive result. In our study, 2 swabs were taken, baseline culture (swab 1) was taken within 3 hours of life under aseptic precautions and was similar to a study on cord colonisation and cord separation time based on dry cord care and topical application of 4 % chlorhexidine and breast milk by Lyndog et al.,16 conducted at North India on preterm (≤ 34 weeks). Common organisms isolated in their study were Klebsiella pneumoniae, Acinetobacter baumannii, Enterococci, Streptococcus and Staphylococcus. Common organisms identified in our study were MSSA, MRSA, Pseudomonas species, CoNS species, Enterobacter species, Klebsiella species, Citrobacter species and Acinetobacter species. These isolated microorganisms are in accordance with other study.17,18 These organisms were presented by other authors as well.19 Ozdemir et al., who evaluated the effect of different antiseptics on cord separation time, also showed that chlorhexidine application was the most effective agent in decreasing colonization, as it significantly increased cord separation time.20 In a study by Azza A et al.,21 2 swab samples were taken, baseline swab was taken soon after birth within 3 hours of life and 2nd swab on third day of life.
In our study, the base line swab (taken within 3 hours of life) of dry cord group had 38.9% growth and that in chlorhexidine group had 1.4% growth. Even though the base line swab in the chlorhexidine group was also taken as in dry cord care group, bacterial colonisation was high in dry cord care group. The second swab colonisation was found in 81.9% and 12.5% in dry cord care group and 4% chlorhexidine group, respectively and the colonisation was statistically significant between the 2 cord care regimen. There were no infections noted in our study and this is similar to many studies.
Developing countries uses different home strategies to keep cord clean. To mention few are use of alcohol, silver sulfadiazine, povidone-iodine, Eau de Dalibour, olive oil, sunflower oil and milk.22 Although the use of antibacterial agents can reduce cord infections, it can also cause the growth of resistant bacteria and increase the risk of neonatal infections.23
Another most important issues after birth is bathing and cleansing of babies. But very limited guidelines are available for skin health. In different countries with various cultures, use/non-use of bathing of neonates on the first days of birth, the best time of the first bath, use of soaps, and bathing intervals are different. A study conducted by Siroosbakht S et al.,24 noticed:“ bathing with or without cleaner were safe and no difference in rate and type of microbial culture in umbilical cord was seen; however, the cord separation time was shorter in dry-cord no bath subjects
As mentioned above, the umbilical cord is a good place for bacterial growth. The recommendation of the World Health Organization is “dry cord care” and the non-use of any agents. But Considering the antibacterial effect of Chlorhexidine over dry cord care, it can be recommended to use in newborns and also to educate the caretakers on its importance and superiority over dry cord care in prevention of infection and mortalities.25
One of the limitations of the study could be the sample size considering the population of India, and also, in this study, only two methods were compared. Therefore, further research can be carried out comparing different commonly used methods commonly used for cord care in a large population.
Use of 4% chlorhexidine is effective in reducing colonization of bacteria and infection. Umbilical cord colonisation is more in dry cord care compared to topical application of 4% chlorhexidine; however, both the cord care method did not result in infections.
ACKNOWLEDGMENTS
None.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORS’ CONTRIBUTION
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
FUNDING
None.
DATA AVAILABILITY
All datasets generated or analyzed during this study are included in the manuscript.
ETHICS STATEMENT
This study was approved by the Institutional Ethics Committee, Kasturba Medical College, Mangalore, India, with reference number IEC KMC MLR 10-19/494.
INFORMED CONSENT
Written informed consent was obtained from the participants before enrolling in the study.
- Kumar P, Singhal N. Mapping neonatal and under-5 mortality in India. Lancet. 2020;395(10237):1591-1593.
Crossref - Stoll BJ. The global impact of neonatal infection. Clin Perinatol. 1997;24(1):1-21.
Crossref - Dramowski A, Pillay S, Bekker A, et al. Impact of 1% chlorhexidine gluconate bathing and emollient application on bacterial pathogen colonization dynamics in hospitalized preterm neonates-A pilot clinical trial. EClinicalMedicine. 2021;37:100946.
Crossref - Adamu A, Onankpa BO, Jega MR, et al. Determinants of umbilical cord care practices among mothers of neonates admitted into special care baby unit of Usmanu Dan Fodiyo University Teaching Hospital, Sokoto, Nigeria. International Journal of Contemporary Medical Research. 2021;8(4):D5-D10.
Crossref - Teferi M, Teferi M, Ayalew A. Prevalence of new born care practice and its associated factors among women who gave birth in the last one year in Adigrattown, Adigrat, Tigray, Ethiopia, 2018/19. Archives of Community Medicine and Public Health. 2020;15;6(1):091-101.
Crossref - Shang Y, Sun Y. Comparison of the effectiveness of different umbilical cord care in infants:A protocol for systematic review and network meta-analysis. Medicine (Baltimore). 2019;98(6):e14440.
Crossref - Ara L, Al Amin M, Billah W, et al. Effectiveness of social and behavioral change communication intervention to promote the use of 7.1% chlorhexidine for umbilical cord care in hard-to-reach rural Bangladesh:A mixed method study. J Glob Health. 2021;11:104006.
Crossref - Udosen IE, Olaoye T, Okondu E, Udosen GE, Amaechi D. Knowledge and attitude of nursing mothers towards umbilical cord care in Calabar Metropolis, Cross River State. Asian Journal of Case Reports in Medicine and Health. 2019;2(1):1-6.
Crossref - Shwe DD, Afolaranmi TO, Egbodo CO, Musa J, Oguche S, Bode-Thomas F. Methylated spirit versus chlorhexidine gel:A randomized non-inferiority trial for prevention of neonatal umbilical cord infection in Jos, North-Central Nigeria. Niger J Clin Pract. 2021;24(5):762-769.
Crossref - Mekonnen M, Estifanos A, Gebremariam M, Biru Y. Effect of Topical Application of Human Breast Milk, Chlorhexidine and Dry Cord Care on Neonatal Umbilical Cord Separation Time and Rate of Cord Infection:Cluster Randomized Trial. Research square. 2020.
Crossref - World Health Organization. Newborns:reducing mortality. 2019. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
- Shen J, Shen M, Jin A. Application of breast milk smears in umbilical care of full-term newborn. Biotechnology and Genetic Engineering Reviews. 2023;6:1-1.
Crossref - WHO Recommendations on Postnatal Care of Mother and Newborn. Geneva:World Health Organization. 2013.
- Jayakody H, Abeysena C. Chlorhexidine for umbilical cord care of the newborn:summary of evidence and its application in Sri Lanka. Journal of the College of Community Physicians of Sri Lanka. 2019;25(3):126-130.
Crossref - Gelano TF, Bacha YD, Abate D. Effect of chlorhexidine cord application on prevention of neonatal sepsis in developing countries:Systematic review and meta-analysis. Int J Health Sci. 2019;13(1):40-51.
- Lyngdoh D, Kaur S, Kumar P, Gautam V, Ghai S. Effect of topical application of human breast milk versus 4% chlorhexidine versus dry cord care on bacterial colonization and clinical outcomes of umbilical cord in preterm newborns. Acad J Ped Neonatol. 2017;5(5):555730.
Crossref - Mullany LC, Shah R, El Arifeen S, et al. Chlorhexidine cleansing of the umbilical cord and separation time:A cluster-randomized trial. Pediatrics. 2013;131(4):708-15.
Crossref - Akyildiz D, Coban A. How the Clamping Distance of the Umbilical Cord affects Microbial Colonization and Cord Separation Time: A Randomized Trial. Puerto Rico Health Sciences Journal. 2023;6;42(1):50-56.
- AM Armanian, B Barekatain, N Salehimehr, et al. Comparison of topical breast milk versus dry cord care on umbilical cord separation, complications and cord colonization, Research Square, Version 1; 05 May 2020 (Preprint).
Crossref - Ozdemir H, Bilgen H, Topuzoglu A, et al. Impact of different antiseptics on umbilical cord colonization and cord separation time. J Infect Dev Ctries. 2017;11(02):152-157.
Crossref - Abd El-Hamid AA, El-Fadil NA, Azzam HF. Effect of two different cord care regimens on umbilical cord stump separation time among neonates at Cairo university hospitals, Department of maternal and newborn health nursing. J Am Sci. 2011;7(12):920-926.
- Walsh S, Norr K, Sankar G, Sipsma H. Newborn cord care practices in Haiti. Glob Public Health. 2015;10(9):1107-1117.
Crossref - Siroosbakht S, Rezakhaniha B. A Survey of Pediatricians’ Views and Practices Regarding Parents’ Request for Prescribing Antibiotics:A Qualitative Study. Arch Pediatr Infect Dis. 2019;7(3):e91217.
Crossref - Siroosbakht S, Aarabi N, Rezakhaniha B. Bathing or Not Bathing:Which Is Better for Umbilical Cord Separation Time and Bacterial Colonization in Neonates?. Arch Pediatr Infect Dis. 2021;9(2):e104100.
Crossref - Turyasiima M, Nduwimana M, Kiconco G, et al. Bacteriology and antibiotic susceptibility patterns among neonates diagnosed of omphalitis at a tertiary special care baby unit in western uganda. Int J Pediatr. 2020.
Crossref
© The Author(s) 2023. Open Access. This article is distributed under the terms of the Creative Commons Attribution 4.0 International License which permits unrestricted use, sharing, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.