ISSN: 0973-7510
E-ISSN: 2581-690X
On July 23, 2022 the World Health Organization (WHO) has announced the Monkeypox disease (MPXD) as a worldwide public health issue. This study conducts a systematic review and meta-analysis to determine the overall case fatality rate (CFR) of MPXD worldwide during 1970–2022. The tenure-tracked MPXD outbreaks associated with CFR were calculated based on available published data from six different periods (i.e., 1970-79, 1980-89, 1990-99, 2000-09, 2010-19, and 2000-2022). A total of 229 peer-reviewed accessible articles were investigated, of which, 17 articles met the inclusion and exclusion criteria. Most of the studies on MPXD CFR were published in the Democratic Republic of the Congo (DRC) providing 47% of data for the current meta-analysis. The overall pooled CFR of MPXD was 4.14% (range: 0.62% – 9.51%) during 1970–2022. In this study, total of 379 death cases were found from published MPXV based research articles where the pooled estimate CFR was 1.87%. The pooled CFR was higher during the earlier outbreak of the MPXD such as 10.71% in 1970-1979. With the progress of time, the CFR from MPXD followed a decreasing trend and reached 5.38% in 1980-1999 and 4.45% in 2000-2022. Young male children aged< 10 years were found to experience the worst outcome with a CFR of >73.0%. This is the first meta-analysis using 52 years of data which indicates that the CFR of MPXV is decreasing from previous years. The findings of this meta-analysis might be paramount for the policymakers to tackle MPXD and minimize the overall CFR of MPXD through strategic actions.
Monkeypox Disease (MPXD), Monkeypox Virus (MPXV), Zoonotic Disease, Case Fatality Rate (CFR), Systematic Review, Meta-analysis
Amid the ongoing COVID-19 pandemic that has caused severe disruptions to global health, economics, and communities due to widespread infection and the emergence of multiple new variants,1-4 the world is now facing a new threat due to the re-emergence of another zoonotic infectious disease, the Monkeypox disease (MPXD).5 Since May 2022, MPXD cases have been reported in many countries in Europe, North America, Asia, and Africa.6 The ongoing outbreaks and rapid spread of MPXD in more than 115 countries are observed as the largest spread of this virus.7 The case fatality rate (CFR) of MPXD can inform specific interferences and the public health scenario of this virus; the ratio of confirmed death patients and diagnosed positive patients number which is converted as a percentage.8
Monkeypox virus (MPXV) is an encapsulated, double-stranded (ds) deoxyribonucleic acid (DNA) virus, a member of the Orthopoxvirus genus and Poxviridae family together with the smallpox virus.9,10 Smallpox, caused by the smallpox virus, has been eradicated with an effective vaccinia virus-based vaccine in 1980.11 MPXD, however, has resurfaced over periods in tropical rainforest regions in Central and West Africa, with the majority of cases reported from the Democratic Republic of the Congo.12 Historically, there are two clades of MPXV which are the West African (WA) clade and the Congo Basin (CB) clade.13 However, a newly proposed clade MPXV Clade 3 has been identified, which originated from the 2017-to-2019 and the most recent 2022 outbreak.14 The CFR is higher in the CB clade (CFR up to 11%) compared to the WA clade (CFR) <1%).15 The MPXD spreads by inhalation or contact with bodily fluids, wounds, lesions, or infected surfaces such as bedding and clothing.16,17 However, up to 30% of all MPXV infections are asymptomatic.18 MPXD is less severe compared to the smallpox virus with a mortality rate is less than 10%.19
To understand disease epidemiological characteristics, there are two key factors such as R0 (reproduction numbers) and CFR (Case fatality rate).20,21 Analysis of CFR of MPXV will assist to find out the epidemiological pattern.22-24 It remains as an important tool to express the fatality of the disease.25-27 The CFR of MPXD can inform specific interferences and the public health scenario of this virus; the ratio of confirmed death patients and diagnosed positive patients number which is converted as a percentage.8 The children are more vulnerable to MPXD and thus, the severity or fatality of MPXD is related to patient conditions and comorbidities. The CFR of MPXD has been reported to range from 0 to 11 % in the general population and has been found higher among young children. However, in recent times, the CFR of MPXD has been around 3–6%.12
The CFR estimation of infectious diseases has many drawbacks such as the reporting period for case diagnosis.28-30 The most important limitation of a CFR calculation is the detection of true cases using active surveillance or testing.31 As MPXV infection is self-limiting with similar clinical characteristics of chickenpox, people usually do not test the infection although the severe cases are more likely to reach health settings and being diagnosed.32 Nonetheless, the lack of available diagnostics made it difficult to diagnose.27,33 Thus, MPXD has been under-reported and under-tested in the communities which leads to a relatively lower denominator resulting in a higher CFR estimation.34
To overcome these limitations and biases of the CFR calculation, in this study, we estimate the average CFR for each study period (e.g., for 1970-1979, 1980-1989, 1990-1999, 2000-2909 and 2010-2019, and onwards up to 2022).35 This review based study aimed to present a systematic review and meta-analysis of the published articles to provide comprehensive updated information on CFR of MPXD. We further studied the current trend of MPXV infection throughout the world to predict and identify countries having the highest incidence of MPXD cases.36
The current systematic review and meta-analysis scrutinized the published MPXD CFR data obtained from previous research publications using previously published search. We used the standard method of the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA) 2009 for conducting this review study.37
Search strategy
Based on the inclusion criteria, the search strategies were operationalized. We searched the Web of Science, PubMed, Google Scholar, and Crossref databases for articles published up to October 2022.38 The search process has been focused on the following terms: (CFR or case fatality rate) and (monkeypox disease or monkeypox virus). We used the following keywords for all the databases: (“monkeypox disease” OR “MPXD” OR “monkeypox virus” OR “MPXV” OR “monkeypox”) AND (“case fatality rate*” OR “case-fatality rate*” OR “case fatality ratio*” OR “CFR” OR “CFRs” OR “case fatality risk*” OR “case-fatality risk*”). The documents’ titles, abstracts, and keywords have been scrutinized throughout the present study. Furthermore, other characteristics of the articles were under precise attention to be chosen, such as having an acceptable quality level and being peer-reviewed; however, the reports, editorial materials, letters, and opinions written only in English were considered. The present research has included the papers published on MPXV, MPXD, and CFR only. The search process has mainly concentrated on reading the critical sections of papers, such as titles and abstracts. The significant challenges in the following purification process were the ambiguity in papers’ titles, keywords, abstracts, and their topic incorporation. However, some addressed the environment and included “MONKEYPOX” or its synonyms. The situation was assigned to a temporal relationship with the MPXD crisis rather than evaluating its CFR impacts. During the data cleanup, some generic terms such as human, humans, article, and study were removed. By eliminating uninformative terms, we improved the publications’ relationship, which positively affected the clustering of the results.11
Data selection criteria
The published research articles were selected on the basis of reported CFR of MPXD patients. The inclusion criteria for published studies were i) laboratory diagnosis of positive MPXD patients; ii) death cases confirmed with MPX infection; iii) considered all countries in the world, all age-groups; and the articles published in the English language. In this meta-analysis study, authors avoided the articles if they were: archive articles, pre-prints (e.g., articles from bioRxiv, Research square, SSRN, and Medrxiv), review-based articles, letters to editorials and different case reports, editorials, short communications, and specific groups with children, male, female, or pregnant women. All the used data from the scrutinized articles is available in Table S1.
Data filtering
Excluding all the duplicate and unrelated articles, two authors blindly assessed the full published articles after checking the article titles and abstracts considering specific criteria. The co-authors assisted to resolve any conflict in this procedure of paper searching for MPXD case fatality. 95% confidence intervals (CIs) were computed for CFR using the Clopper-Pearson exact method. A standard Microsoft excel form was used for extracting all the required information from articles including article title, authors name, published year, journal name, DOI number, name of the publisher, country name, study area, study period, sample size, case fatality rates. We defined MPXD as a disease caused by the MPXV. The CFR is the ratio of MPXD-confirmed death cases and MPXV-positive cases.
Descriptive studies
Preliminary searches identified 249 articles on the assigned searching criteria during 1970 to October, 2022 across all of the four databases (Web of Science= 30, PubMed= 39, Crossref= 31 and Google Scholar= 149) (Figure 1). Following all the exclusion and inclusion criteria and the standard procedure, we extracted only 17 published articles (Google Scholar = 10, PubMed = 4 and Web of Science = 3). Among the finalized 17 published research articles maximum (47%) were published in the year between 2010-2022, followed by 11% during 2000-2009, 11% during 1990-1999, and 29% during 1980-1989 (Table 1). The selected 17 articles were published from six different countries including DRC (n=8), Nigeria (n=3), Republic of the Congo (n = 3), and one article from Central African Republic, South Sudan, and United Kingdom (each). DRC is the country where major research on MPXD related CFR were carried out throughout the study period, and thus, contributed 47% of articles in this review study (Table 1).
Table (1):
Characteristics of included studies in the meta-analysis for CFR.
Author/Study |
Location |
Study Period |
CFR |
Confirmed Cases |
Deaths |
|---|---|---|---|---|---|
Breman et al., 1980 |
Democratic Republic of the Congo |
1970 – 1979 |
21.0 |
38 |
8 |
Breman et al., 1980 |
Nigeria |
1970 – 1979 |
0.0 |
1 |
0 |
Doshi et al., 2019 |
Republic of the Congo |
January 2017 – 5 April 2017 |
13.6 |
22 |
3 |
Formenty et al., 2010 |
South Sudan |
September 2005 – December 2005 |
0.0 |
19 |
0 |
Hutin et al., 1997 |
Democratic Republic of the Congo |
1996 – 1997 |
3.7 |
81 |
3 |
Ita et al., 2019 |
Nigeria |
5th October – 7th November 2017 |
0.0 |
15 |
0 |
Jezek et al., 1986 |
Democratic Republic of the Congo |
1981 – 1986 |
20.0 |
5 |
1 |
Jezek et al., 1988 |
Democratic Republic of the Congo |
May 1983 – July 1983 |
9.8 |
338 |
33 |
Jezek et al., 1988 |
Democratic Republic of the Congo |
1981 – 1985 |
9.0 |
91 |
8 |
Learned et al., 2005 |
Republic of the Congo |
April 2003 – June 2003 |
9.0 |
11 |
1 |
Mandja et al., 2022 |
Republic of the Congo |
2000 – 2015 |
1.52 |
19273 |
292 |
Meyer et al. 2002 |
Democratic Republic of the Congo |
February 2001 – August 2001 |
16.1 |
31 |
5 |
Mwanbal et al., 1997 |
Democratic Republic of the Congo |
February 1996 – February 1997 |
3.3 |
92 |
3 |
Nakouné et al., 2017 |
Central African Republic |
December 2015 – February 2016 |
23.1 |
13 |
3 |
Nolen et al., 2016 |
Democratic Republic of the Congo |
July 2013 – Dec 2013 |
25.6 |
39 |
10 |
Vaughan et al., 2020 |
United Kingdom |
September 2018 |
0.0 |
1 |
0 |
Yinka-Ogunleye et al., 2019 |
Nigeria |
2017 – 2019 |
5.0 |
181 |
9 |
Figure 1. PRISMA (Preferred Reporting Items for Systematic Review and Meta-Analysis) flow diagram of the systematic review. Case Fatality Rate is abbreviated as CFR (CFR = Case Fatality Rate)
Analysis of case fatality rate (CFR)
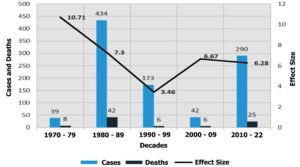
The pooled CFR for MPXD in the random-effects model was 4.14% (95%CI: 0.62%, 9.51%). The pooled CFR of MPXD in different decades was 10.71% (95%CI: 0.15, 29.31) in 1970-1979, 5.38% (95%CI: 2.32, 9.31) in 1980-99, and 4.45% (95%CI: 0.10, 12.36) in 2000-2022 There was a significant variation of CFR between decades (P=0.05) (Figure 2, Table 2). The lowest CFR (4.14%) was reported in 2000-2022, while the highest CFR 10.71% was found during 1970- 1979 (Figure 2). There was a 1.21-fold decreasing trend of CFR during 1980- 1999 and 2000- 2022(i.e., from 5.38 to 4.14%) (Figure 2). Beyond 1999, again there was a slight decreasing to 2022 (Figure 2).
Table (2):
Effect size and test of heterogeneity for the case fatality rate (CFR) by decades.
| Statistics | Decade | Test for Subgroup differences | Overall | ||
|---|---|---|---|---|---|
| Up to 1979 | 1980-99 | 2000-19 | |||
| Effect Size (95% CI) | 10.71 (0.15, 29.31) | 5.38 (2.32, 9.31) | 4.45 (0.10, 12.36) | 5.94 (p-value = 0.05) |
4.14 (0.62, 9.51) |
| I2 statistic | – | – | – | 89.51% | |
| Cochran’s Q statistics | – | – | – | 152.47 | |
| n (sample=17) | 2 | 5 | 10 | 17 | |
Figure 2. Monkeypox disease (MPXD) cases and case fatality rates (CFRs) throughout the study period (i.e., from 1970 to 20202). No published article on MPXD CFR was found during 2020 to 2022, and thus not included in the graph
Figure 3. The pooled case fatality rate (CFR) of Monkeypox disease (MPXD) according to gender and age groups. (A) The pooled CFR of MPXD in according to gender (male and female), and (B) The pooled CFR of MPXD in according to age groups (i.e., < 10 years of age, 10-20 years of age and > 20 years of age)
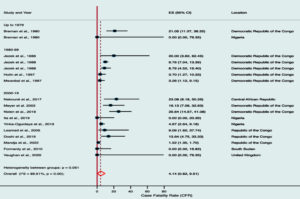
Case fatality rate based on gender and age
Data on the gender and age of confirmed cases of MPXD, and/or possible CFR are presented in Figure 3. The distribution of CFR in MPXD based on gender and age were available in nine studies. A total of 379 deaths were recorded in these studies, and the pooled CFR in these studies was 1.87%. The country-wise CFR estimation of MPXD cases revealed the highest CFR in the Central African Republic (23%) followed by DRC (10%), Nigeria (5%) and Republic of Congo (2%) (Table 2). All the 379 deaths from MPXD reported in this study occurred in the African countries (which had>20000 confirmed cases of MPXD). However, only one death case was found to be reported outside the African countries (i.e., United Kingdom). The gender and age-related differences in the male to female MPXD-associated deaths and corresponding CFR is depicted in Figure 3. The pooled CFR in males was 73.33% (95%CI: 15.51, 80.60) whereas 26.67% (95%CI: 5.76, 30.44) was estimated for females (Figure 3A). According to this study results it is established that younger children (<10 years) affected severely by this virus, and the CFR was 76.47% (95% CI: 8.56, 92.30)(Figure 3A). People aged between 10-20 years however had the lowest pooled CFR (7.35%) (Figure 3B).
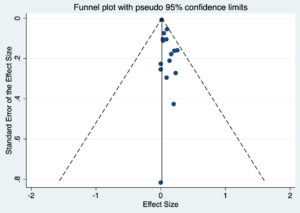
Risk of bias
It is well established that all estimates obtained from modeling studies are considered to be at a high risk of bias due to the heterogeneity and difficulty in rating respective studies for accuracy. Therefore, to avoid risk of bias we performed random effect analysis. The result from the random effects meta-analysis is also presented in Figure 4. Overall, the aggregated estimate (ES) across all 15 studies of the five periodic subgroups indicated an overall CFR of 4.14% (95% CI 0.62, 9.51). Heterogeneity between studies was found to be moderately high (I2 statistic = 89.51% and Cocharn’e Q statistic = 152.47, P = 0.05) (Figure 5).
Figure 4. The Forest plot of estimated case fatality rate (CFR) values of Monkeypox disease (MPXD) in different sub-groups (decade-based) based on random-effects model
The recent re-emergence of the MPXD in multiple non-endemic countries beyond African territories has created an international public health emergency.39 In this systematic review 17 articles identified on CFR of MPXD. We identified one article on MPXD CFR published in 2020 from the United Kingdom, complying our search criteria.40 Our review identified total 379 deaths confirmed with MPXV infection giving rise to crude CFR of 1.87% while the random effect model estimated an overall pooled CFR of 4.1%. The males had higher risk of dying from MPXV (765 vs. 26.7%) while children belonged to <10 years had the greatest risk of dying from MPXV infection (76.4%). Central African Republic (23%), DRC (10%), and Nigeria (5%) experience a higher CFR.41
This study showed a divergence in the MPXV CFR in different time frame that indicates a higher CFR at the very beginning of the first emergence of MPXD (highest CFR of 10.71% during 1970-1979).7,23,42,43 Later on, there was a gradual declining ratio up to 1999. With the increasing number of MPXD outbreak in recent years in Africa and outside of Africa,15 we also found an increasing rate of CFR in the last two decades (from 2000 to onwards).44 The reason why CFR cases has changed in different study period is not clear to us, but the development on detection technology, increase awareness about the disease and the development in reporting system might have an effect.
So far, majority of MPXD outbreaks were recorded in African (primarily West and Central) countries,45 therefore, we found the highest number of published articles in the DRC and Nigeria. We found that MPXD was more prevalent in four African countries (e.g., DRC, Nigeria, Central African Republic, and South Sudan) and as well in the United Kingdom. The country-wise CFR estimation revealed the highest CFR of MPXD in the Central African Republic followed by DRC and Nigeria. Our analysis revealed that male cases of MPXD occurred more frequently than female cases in which gender information were available. Moreover, most deaths due to MPXD infection found in this review are among male patients with concurrent increased CFR. In a recent retrospective observational study in the UK,46 higher CFR of human MPXD has been reported in males compared to females supporting our review findings. Besides CFR differences in gender, the present meta-analysis revealed a significant difference in CFR in the people at age group younger than 10 years and older (> 20 years). Our systematic review and meta-analysis analysis shows that in throughout the study period (1970–2022), MPXD was primarily a disease of young children, with highest pooled CFR (76.47%) at an age presentation of 1–9 years old (< 10 years old). Regarding age at death in MPXD cases, 100% of deaths were in children <10 years of age corroborating with the results of many of the previous studies.15 These data appear to be consistent with the global intensified spread of MPXD infections and concurrent severity among children. Interestingly, lowest pooled CFR (7.35%) of MPXD were found in people at 10 to 20 years of age.47
In a systematic review and meta-analysis of global MPXV case hospitalization rate (CHR) is observed as 49.8% (28.2-74.0, I2 81.4%), 21.7% (7.2-52.1, I2 57.7%) during outbreak time and 5.8% (3.2-9.4, I2 92.4%) during the pre-2017, 2017-2021, and 2022 outbreaks, respectively. Case fatality rate (CFR) was found as 0.03% (0.0-0.44, I2 99.9%) from 19 studies out of 259 including 7553 reported case and 555 hopitalized cases.48,49
We also found moderately high (36.0 to 59.0%) heterogeneity in CFR among the selected studies using two different statistical analyses; I2 statistic and Cocharn’e Q statistic) corroborating with the results of several the earlier studies (48). In several recent meta-analysis on the global case fatality rate of Ebola and COVID-19 higher heterogeneity in CFR among the selected studies were reported supporting our present findings.1,4,48 Thus, highly organized and developed, depth research analyses are needed to find out the effects various factors related with fatality of MPXD. Although, there is very limited information on incubation time, the disease severity, host immunity, and the existence of the disease are all determined by the route of viral entry, with infection via wild animal bites taking less time than others. In order to better understand how this virus spreads, additional research is needed about natural animal reservoirs and the evolving and changing epidemiology of the virus.24,25,50
Limitations
Overall, 17 relevant articles were screened for comprehensive data extraction. However, there are also some limitations hardly could avoid. So this is an important limitation. Research articles focusing MPXV might be published in French language as DRC is a French speaking countries and this study has no such studies.51 The limitations of our current study are lack of enough published articles from a varying area of the world, and estimated CFR for these areas might not proper.52 The original scenario of CFR and MPXD may differ due to awareness of people about the disease, so on which stage people visit doctor, clinical investigation methodology, registration systems, variability individual migrations, different environment, and mobility, behavior and habits, economic and lifestyle, and cultural conditions––which may affect MPXD mortality and incidence by acting as confounders.53-54
Monkeypox is a re-emerging viral disease, which spread in multiple countries with a potential to become an epidemic. Seventeen out of 229 peer-reviewed articles were selected for this meta-analysis based on the rigid inclusion-exclusion criteria. The pooled CFR of MPXD was higher (> 10.0%) in the first decade (1970-1979) of its emergence in 1970. We also found an increasing trend of CFR (> 6.0%) during last two decades (1990-2022). The pooled CFR of MPXD was higher in African countries (e.g., Central African Republic, DRC and Nigeria) compared to non-African countries. Young male children of at < 10 years of age were most susceptible to MPXD severity, with higher deaths and concurrent pooled CFR (> 73.0%) compared to other age groups. The random-effects model showed a CFR of more than 4.0%. Our study emphasizes that CFR in MPXD cases is not a fixed or static value, rather it is in a further increasing trend (since 1999) in the recent years. We observed that MPXD related CFR could vary according to study periods and demographic characters (region, country, age, gender etc.). The findings of this review will help researchers, academicians, health professionals, and policymakers to minimize the fatality rates and risk of MPXD by taking strategic actions and precautions against MPXD. The findings of this comprehensive study could be useful for an appropriate policy decisions to tackle the potentially epidemic MPXD.
Additional file: Additional Table S1.
ACKNOWLEDGMENTS
None.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORS’ CONTRIBUTION
MAI conceptulized the study. TA, STAN, MNY extracted data and helped in analysis. MZH analyzed the data. MZH, MNH, AT, HH, KD, TI, PB drafted and edited the manuscript. MAI supervised the project. All authors read and approved the final manuscript for publication.
FUNDING
None.
DATA AVAILABILITY
All datasets generated or analyzed during this study are included in the manuscript and/or in the supplementary files.
ETHICS STATEMENT
Not applicable.
- Ahmed F, Aminul Islam M, Kumar M, et al. First detection of SARS-CoV-2 genetic material in the vicinity of COVID-19 isolation centre through wastewater surveillance in Bangladesh. medRxiv. 2020;2020.09.14.20194696.
Crossref - Islam MA, Haque MA, Rahman MA, et al. A Review on Measures to Rejuvenate Immune System: Natural Mode of Protection Against Coronavirus Infection. Front Immunol. 2022;13:837290.
Crossref - Islam MA, Marzan AL, Sydul MI, et al. Sex-specific epidemiological and clinical characteristics of COVID-19 patients in the southeast region of Bangladesh. MedRxiv. 2021.
Crossref - Jakariya M, Ahmed F, Islam MA, et al. Wastewater-based epidemiological surveillance to monitor the prevalence of SARS-CoV-2 in developing countries with onsite sanitation facilities. Environ Pollut. 2022;311:119679.
Crossref - Sallam M, Al-Mahzoum K, Dardas LA, et al. Knowledge of Human Monkeypox and Its Relation to Conspiracy Beliefs among Students in Jordanian Health Schools: Filling the Knowledge Gap on Emerging Zoonotic Viruses. Medicina. 2022;58(7):924.
Crossref - WHO. Multi-country monkeypox outbreak: situation update. Available from: https://www.google.com/search?client=firefox-b-d&q=WHO.+Multi-country+monkeypox+outbreak%3A+situation+update. Accessed on: 20 December,2022
- Chakraborty S, Mohapatra RK, Chandran D, et al. Monkeypox vaccines and vaccination strategies: Current knowledge and advances. An update – Correspondence. Int J Surg. 2022;105:106869.
Crossref - Ahammed T, Anjum A, Rahman MM, Haider N, Kock R, Uddin MJ. Estimation of novel coronavirus ( <scp>COVID</scp> -19) reproduction number and case fatality rate: A systematic review and meta-analysis. Heal Sci Reports. 2021;4(2):e274.
Crossref - Chandran D, Dhama K, KM AM, et al. Monkeypox : An Update on Current Knowledge and Research Advances. J Exp Biol Agric Sci. 2022;10(2320):679-688.
Crossref - Giorgi J, Bader G, Wang B. A sequence-to-sequence approach for document-level relation extraction. Proceedings of the 21st Workshop on Biomedical Language Processing. Stroudsburg, PA, USA: Association for Computational Linguistics; 2022:10-25.
Crossref - Mauldin MR, McCollum AM, Nakazawa YJ, et al. Exportation of Monkeypox Virus From the African Continent. J Infect Dis. 2022;225(8):1367-1376.
Crossref - Adler H, Gould S, Hine P, et al. Clinical features and management of human monkeypox: a retrospective observational study in the UK. Lancet Infect Dis. 2022. https://linkinghub.elsevier.com/retrieve/pii/S1473309922002286
- Mohapatra RK, Tuli HS, Sarangi AK, et al. Unexpected sudden rise of human monkeypox cases in multiple non-endemic countries amid COVID-19 pandemic and salient counteracting strategies: Another potential global threat? Int J Surg. 2022;103:106705.
Crossref - Luna N, Ramiirez AL, Munoz M, et al. Phylogenomic analysis of the monkeypox virus (MPXV) 2022 outbreak: Emergence of a novel viral lineage? Travel Med Infect Dis. 2022;49:102402.
Crossref - Bunge EM, Hoet B, Chen L, et al. The changing epidemiology of human monkeypox-A potential threat? A systematic review. Gromowski G, editor. PLoS Negl Trop Dis. 2022;16(2):e0010141.
Crossref - Jain N, Lansiaux E, Simanis R. The new face of monkeypox virus: an emerging global emergency. New Microbes New Infect. 2022;47:100989.
Crossref - Barnewall RE, Fisher DA, Robertson AB, Vales PA, Knostman KA, Bigger JE. Inhalational monkeypox virus infection in cynomolgus macaques. Front Cell Infect Microbiol. 2012;2:117.
Crossref - Zumla A, Valdoleiros SR, Haider N, et al. Monkeypox outbreaks outside endemic regions: scientific and social priorities. Lancet Infect Dis.. 2022;22(7):929-931.
Crossref - Reynolds MG, Doty JB, McCollum AM, Olson VA, Nakazawa Y. Monkeypox re-emergence in Africa: a call to expand the concept and practice of One Health. Expert Rev Anti Infect Ther. 2019;17(2):129-139.
Crossref - Islam A, Hossen F, Rahman A, et al. An opinion on Wastewater-Based Epidemiological Monitoring (WBEM) with Clinical Diagnostic Test (CDT) for detecting high-prevalence areas of community COVID-19 Infections. Curr Opin Environ Sci Heal. 2022;100396.
Crossref - Islam A, Rahman A, Jakariya, et al. A 30-day follow-up study on the prevalence of SARS-COV-2 genetic markers in wastewater from the residence of COVID-19 patient and comparison with clinical positivity. Sci Total Environ. 2022;159350.
Crossref - Chakraborty S, Chandran D, Mohapatra RK, et al. Marburg Virus Disease – A Mini-Review. J Exp Biol Agric Sci. 2022;10(4):689-696.
Crossref - Chakraborty C, Bhattacharya M, Sharma AR, et al. Deep learning research should be encouraged for diagnosis and treatment of antibiotic resistance of microbial infections in treatment associated emergencies in hospitals. Int J Surg. 2022;105:106857.
Crossref - Haque MA, Wang F, Chen Y, et al. Bacillus spp. Contamination: A Novel Risk Originated From Animal Feed to Human Food Chains in South-Eastern Bangladesh. Front Microbiol. 2022;12:783103.
Crossref - Hossain FE, Islam S, Islam MA, Islam S, Ahmed F. Detection of virulence genes of APEC (avian pathogenic Escherichia coli) isolated from poultry in Noakhali, Bangladesh. Bioresearch Commun. 2021;7(1):967-972.
Crossref - Sakib MMH, Nishat AA, Islam MT, et al. Computational screening of 645 antiviral peptides against the receptor-binding domain of the spike protein in SARS-CoV-2. Comput Biol Med. 2021;136:104759.
Crossref - Roy S, Bhowmik DR, Begum R, et al. Aspirin attenuates the expression of adhesion molecules, risk of obesity, and adipose tissue inflammation in high-fat diet-induced obese mice. Prostaglandins Other Lipid Mediat. 2022;162:106664.
Crossref - Hossain M, Saiha Huq T, Rahman A, et al. Novel mutations identified from whole-genome sequencing of SARS-CoV-2 isolated from Noakhali, Bangladesh. Research Square. 2021.
Crossref - Rakib SH, Masum S, Farhana RA, et al. Design of a Cost-Effective Ultraviolet Disinfection Unit to Minimize the Cross-Contamination of COVID-19 in Transport. International Conference on Advancement in Electrical and Electronic Engineering (ICAEEE). 2022.
Crossref - Rakib SH, Masum S, Patwari MRI, Fahima RA, Farhana A, Islam MA. Design and Development of a low cost Ultraviolet Disinfection system to reduce the cross infection of SARS-CoV-2 in ambulances. International Conference on Electronics, Communications and Information Technology (ICECIT). IEEE. 2021:1-4.
Crossref - Kannan SR, Sachdev S, Reddy AS, et al. Mutations in the monkeypox virus replication complex: Potential contributing factors to the 2022 outbreak. J Autoimmun. 2022;133:102928.
Crossref - Morgan OW, Bramley A, Fowlkes A, et al. Morbid Obesity as a Risk Factor for Hospitalization and Death Due to 2009 Pandemic Influenza A(H1N1) Disease. Sorensen TIA, editor. PLoS One. 2010;5(3):e9694.
Crossref - Jakariya M, Ahmed F, Islam MA, et al. Wastewater based surveillance system to detect SARS-CoV-2 genetic material for countries with on-site sanitation facilities: an experience from Bangladesh. medRxiv.
Crossref - Peiro-Mestres A, Fuertes I, Camprubi-Ferrer D, et al. Frequent detection of monkeypox virus DNA in saliva, semen, and other clinical samples from 12 patients, Barcelona, Spain, May to June 2022. Euro Surveill. 2022;27(28):2200503.
Crossref - Ahmed F, Islam MA, Kumar M, et al. First detection of SARS-CoV-2 genetic material in the vicinity of COVID-19 isolation Centre in Bangladesh: Variation along the sewer network. Sci Total Environ. 2021;776:145724.
Crossref - Thornhill JP, Barkati S, Walmsley S, et al. Monkeypox Virus Infection in Humans across 16 Countries – April-June 2022. N Engl J Med. 2022;387(8):679-691.
Crossref - Bragazzi NL, Kong JD, Mahroum N, et al. Epidemiological trends and clinical features of the ongoing monkeypox epidemic: A preliminary pooled data analysis and literature review. J Med Virol. 2022.
Crossref - Sah R, Humayun M, Baig E, et al. FDA’s authorized “JYNNEOS” vaccine for counteracting monkeypox global public health emergency; an update – Correspondence. Int J Surg. 2022;107:106971.
Crossref - Tambo E, Al-Nazawi AM. Combating the global spread of poverty-related Monkeypox outbreaks and beyond. Infect Dis Poverty. 2022;11(1):80.
Crossref - Saxena SK, Ansari S, Maurya VK, et al. Re-emerging human monkeypox: A major public-health debacle. J Med Virol. 2022.
Crossref - Beig M, Mohammadi M, Nafe Monfared F, Nasereslami S. Monkeypox: An emerging zoonotic pathogen. World J Virol. 2022;11(6):426-34.
Crossref - Dhama K, Chandran D, Chakraborty S, et al. Zoonotic concerns of Marburg virus: Current knowledge and counteracting strategies including One Health approach to limit animal-human interface: An update. Int J Surg. 2022;106:106941.
Crossref - Chakraborty S, Chandran D, Mohapatra RK, et al. Langya virus, a newly identified Henipavirus in China – Zoonotic pathogen causing febrile illness in humans, and its health concerns: Current knowledge and counteracting strategies – Correspondence. Int J Surg. 2022;105:106882.
Crossref - Tutu van Furth AM, van der Kuip M, van Els AL, et al. Paediatric monkeypox patient with unknown source of infection, the Netherlands, June 2022. Euro Surveill. 2022;27(29):1-5.
Crossref - Yong SEF, Ng OT, Ho ZJM, et al. Imported Monkeypox, Singapore. Emerg Infect Dis. 2020;26(8):1826-1830.
Crossref - Ophinni Y, Frediansyah A, Sirinam S, Megawati D, Stoian AM, Enitan SS, et al. Monkeypox: Immune response, vaccination and preventive efforts. Narra J 2022; 2(3):e90.
Crossref - Yuan Y, Cao D, Zhang Y, et al. Cryo-EM structures of MERS-CoV and SARS-CoV spike glycoproteins reveal the dynamic receptor binding domains. Nat Commun. 2017;8:15092.
Crossref - Ghayda RA, Lee KH, Han YJ, et al. The global case fatality rate of coronavirus disease 2019 by continents and national income: A meta-analysis. J Med Virol. 2022;94(6):2402-2413. https://onlinelibrary.wiley.com/doi/10.1002/jmv.27610
- Tiwari A, Adhikari S, Kaya D, et al. Monkeypox outbreak: Wastewater and environmental surveillance perspective. Sci Total Environ. 2023;856:159166.
Crossref - Sobral-Costas TG, Escudero-Tornero R, Servera-Negre G, et al. Human monkeypox outbreak: epidemiological data and therapeutic potential of topical cidofovir in a prospective cohort study. J Am Acad Dermatol. 2022.
Crossref - Tiecco G, Degli Antoni M, Storti S, Tomasoni LR, Castelli F, Quiros-Roldan E. Monkeypox, a Literature Review: What Is New and Where Does This concerning Virus Come From? Viruses. 2022;14(9):1894.
Crossref - Islam MA, Hasan MN, Ahammed T, et al. Association of household fuel with acute respiratory infection (ARI) under-five years children in Bangladesh. Front Public Heal. 2022;10:985445.
Crossref - Islam MA, Sangkham S, Tiwari A, et al. Association between Global Monkeypox Cases and Meteorological Factors. Int J Environ Res Public Health. 2022;19(23):15638.
Crossref - Islam MA, Adeiza SS, Amin MR, et al. A bibliometric study on Marburg virus research with prevention and control strategies. Front Trop Dis. 2022;3:1068364.
© The Author(s) 2022. Open Access. This article is distributed under the terms of the Creative Commons Attribution 4.0 International License which permits unrestricted use, sharing, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.